젊은 근시안에서 동체시력과 동적시력의 특징

초록
젊은 근시환자를 대상으로 동체시력(Dynamic visual acuity, DVA)과 동적시력(Kinetic visual acuity, KVA)의 특징을 알아보고, 안구 인자와 임상 검사 결과들이 동체시력과 동적시력에 미치는 영향을 알아보고자 하였다.
20-32세 사이의 80명 근시안을 대상으로 하였다. 동체시력과 동적시력을 측정하기 전, 나안시력과 구면등가굴절력, 안압을 측정하였고, 광학저간섭성 반사계(optical low coherence reflectometry)를 통해 안축 길이, 각막 두께, 수정체 두께, 전방 깊이, 동공 크기를 측정하였으며, 빛간섭단층촬영(Cirrus high-definition optical coherence tomography)을 시행하여 황반부 두께를 측정하였다. 동체시력 분석기(제작 문장일, 심현석, 김영청)와 동적시력 측정기 AS-4A (KOWA, Tokyo, Japan)를 이용하여 단안과 양안의 동체시력과 동적시력을 각각 측정하였고, 1주 후와 4주 후에 반복하여 측정하였다.
단안시와 양안시 비교에서, 단안 동체시력보다 양안 동체시력이 더 좋았으나 동적시력은 차이가 없었다. 남자가 여자보다 동체시력과 동적시력이 기준일, 1주 후, 4주 후에서 모두 우수하였다. 동체시력은 근시가 낮을수록, 안축 길이가 짧을수록, 동공 크기가 클수록 우수하였고, 동적시력은 근시가 낮을수록, 안축 길이가 짧을수록 우수하였으나 동공 크기와는 관련을 보이지 않았다.
동체시력과 동적시력은 성별, 근시 정도, 안축의 길이, 동공 크기에 따라 차이를 보였다. 동체시력과 동적시력을 측정하고자 할 때 임상적, 안구 생체 요소가 영향을 준다는 것을 고려해야 할 것이다.
Abstract
To investigate the characteristics of dynamic visual acuity (DVA) and kinetic visual acuity (KVA) in young myopic eyes and to investigate the clinical or ocular factors affecting DVA and KVA.
Eighty subjects aged between 20-32 years old were recruited. Before measuring the DVA and KVA, visual acuity, spherical equivalent refractive error, intraocular pressure were measured, and axial length, central corneal thickness, anterior chamber depth, lens thickness, pupil diameter were obtained by optical low coherence reflectometry (Haag-Streit, Köniz, Switzerland) and central subfield thickness, cube volume, cube average thickness parameters of macular were measured using a Cirrus high-definition optical coherence tomography (HD-OCT) device (Carl Zeiss Meditec, Dublin, CA, USA). Monocular and binocular DVA were measured using a dynamic visual acuity analyzer (designed by Jangill Moon, Hyunsuk Shim, and Youngcheong Kim). Monocular and binocular KVA were measured using a kinetic visual acuity meter AS-4A (KOWA, Tokyo, Japan). All measurements were repeated at baseline, 1 week, and 4 weeks.
In comparison between monocular and binocular viewing, binocular DVA was higher than monocular DVA. However, there was no difference in KVA. Men showed higher DVA and KVA than women at baseline, 1 week, and 4 weeks. The lower degree of myopia, shorter axial length, and longer pupil diameter were the higher DVA. Similarly, the lower degree of myopia and shorter axial length were the higher KVA. However, KVA did not show association with pupil diameter.
DVA and KVA may be different by sex, degree of myopia, axial length, pupil diameter. Clinical factors and ocular biometry should be considered when measuring DVA and KVA.
Keywords:
DVA, Dynamic visual acuity, KVA, Kinetic visual acuity, Clinical factor, Myopia, Ocular biometry, Pupil diameter, Axial length키워드:
DVA, 동체시력, KVA, 동적시력, 임상요소, 근시, 안구생체요소, 동공 크기, 안축 길이INTRODUCTION
Dynamic visual acuity (DVA) refers to the ability to discriminate the fine parts of a horizontally moving object during relative motion between the object and the observer. Kinetic visual acuity (KVA) refers to the ability to discriminate the fine parts of an object moving from a distant point towards the subject.[1-3] DVA and KVA are suitable for estimating the visual functions of athletes who continue to pursue a moving ball during their play, so these two parameters have been widely studied to measure the ability to visually discern a moving object in athletes of various sports especially using ball such as baseball, volleyball, and basketball.[1-5]
Winograd reported that college baseball players showed better visual efficiency and better stereoacuity than the general public and students who did not qualify for the team.[6] Rouse et al. also reported that DVA of college baseball players was better than nonathletic students.[7] Laby et al showed that visual acuity, contrast sensitivity, and distance stereoacuity of Los Angeles Dodgers baseball players were better than general public.[4] But all above mentioned studies were conducted without considering the ocular factors such as degree of myopia, gender, axial length and pupil diameter.
Recent technological advances in optical biometry have been achieved by latest introduction of swept-source optical coherence tomography.[8,9] Ocular parameters such as axial length, corneal thickness, anterior chamber depth, lens thickness and pupil diameter can be measured by the swept-source optical coherence tomography, and many studies have been reported that above mentioned ocular parameters can be measured with high repeatability and reproducibility.[10-13] Until now, the most studies[14,15] have considered correlations of KVA and DVA with refractive errors, corrected visual acuity, static visual acuity(SVA), dominant eye and pupil distance(PD), and none of studies have considered the biometric ocular elements provided by optical low coherence reflectometry when analyzing DVA and KVA.
The purpose of this study was to investigate the characteristics of DVA and KVA according to the sex, refractive error, and pupil diameter in young myopic eyes with normal anatomical macular. Also, we investigated if clinical or ocular factors such axial length, affecting DVA and KVA.
MATERIALS AND METHODS
1. Subjects
Healthy volunteers were prospectively and consecutively recruited from September 2014 to July 2015. The subjects were selected from students attending the Chonnam National University Medical School. The participants were informed about the study objectives, and signed informed consent was obtained from all participants. During the enrollment period, 86 subjects were evaluated and 4 subjects were excluded because of prior refractive surgery, 2 subjects were excluded due to follow up loss. Total 80 subjects (male 42, female 38) were enrolled in this study. All subjects underwent complete ophthalmic examination including measurement of best-corrected visual acuity, intraocular pressure (IOP) by Goldmann applanation tonometry, manifest refraction, slit-lamp examination and stereoscopic disc photography and red-free disc photography.
Healthy subjects aged between 20 and 40 years, a spherical equivalent (SE) refractive error between −9.0 and −0.5 diopters (D), astigmatism within ± 2D, monocular best-corrected visual acuity ≥ 20/25, binocular best-corrected visual acuity ≥ 20/20, IOP ≤ 21 mmHg, normal anterior chamber angles, nonglaucomatous ONHs (Optic Nerve Heads) on stereoscopic photographs (an intact neuroretinal rim without peripapillary hemorrhage, thinning, or localized pallor), and absence of any RNFL (Retinal Nerve Fiber Layer) abnormalities on red-free fundus photographs. We excluded subjects with a family history of glaucoma in a firstdegree relative, history of intraocular or refractive surgery, pathologic myopia (patch chorioretinal atrophy, lacquer crack lesions, intrachoroidal cavitations, choroidal neovascularization), other evidence of retinal pathology, or opaque media.
Axial length, central corneal thickness, anterior chamber depth, lens thickness and pupil diameter were measured in a dimly lighted room by optical low-coherence reflectometry (Lenstar; Haag-Streit AG, Koeniz, Switzerland). The central subfield thickness, cube volume, cube average thickness parameters of macular were measured using a Cirrus high-definition optical coherence tomography (HD-OCT) device (Carl Zeiss Meditec). All measurements were done at baseline, 1 week, 4 weeks and performed by the same examiner who was experienced in taking OCT images. A detailed medical history was also recorded for each subject.
DVA was measured using a dynamic visual acuity analyzer (designed by J.I.M, H.S.S, and Y.C.K, Fig. 1), and measured with monocularly (right to left) and binocularly and then KVA was measured in the same order using a kinetic visual acuity meter AS-4A (KOWA, Tokyo, Japan, Fig. 2).
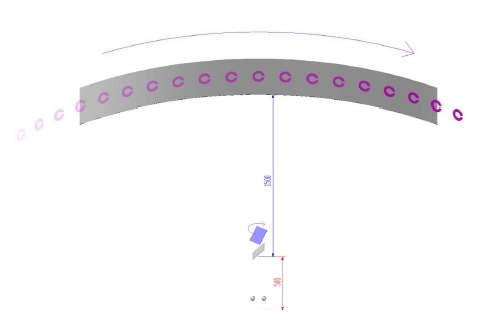
Schematic diagram of dynamic visual acuity analyzer (designed by Jangill Moon, Hyunsuk Shim, and Youngcheong Kim) Radius of curvature and length of arc of screen was 1.5 m, and Landolt-C ring size was 0.05 visual acuity chart with outer diameter 60 mm. When measuring DVA, Landolt-C ring moving from left to right, on the screen 2 m distant from the subject. If subject identified the Landolt-C ring gap, the examiner changed the moving velocity of the Landolt-C ring more faster.
For the measuring DVA, the radius of curvature screen was 1.5 m and visual acuity chart was 0.05 Landolt-C ring. The subjects were directed to put their chins on the chin rest, and their eyes followed the Landolt-C ring moving from left to right, on the screen at a 2 m distant from the subjects. Subjects were not allowed to move or turn their heads during the measurements. Subjects were asked to tell the identified direction of Landolt-C ring. If subject answered wrong direction, the examiner randomly changed the direction with the same speed, and then the subject had two more chances to tell the right answer. Fastest moving velocity of the Landolt-C ring when the subject could identify the ring gap was used for analysis.
For the measuring KVA, the subjects were directed to look through the eyepiece. Black Landolt-C ring in a bright white circular shape would appear in the eyepiece. AS-4A showed the Landolt-C ring moving towards the subjects horizontally from a 50 m distance at a rate of 30 km/hour. Subjects were asked to immediately push the button when they could identify the direction of the ring gap. Landolt-C ring size according to the identification distance was converted to decimal visual acuity and used for analysis (Table 1). The identification of the smaller the Landolt-C ring size, indicates the better KVA.

The conversion chart of kinetic visual acuity according to the identification distance of the Landolt-C ring in the kinetic visual acuity meter
DVA and KVA were measured at base line, 1 week, and 4 weeks by the same examiner. Subjects were asked to respond consecutive three times for each measurement until they get the right answer. The mean value of the three measurements was used in analysis.
SPSS version 18.0 (SPSS Inc., Chicago, IL) was used for all statistical analyses. Baseline characteristics were reported in mean ± standard deviation values. Groups were compared using student t test and pearson’s correlation analysis. P-values < 0.05 were considered statistically significant.
RESULTS AND DISCUSSION
Subject's characteristics are presented in Table 2. The mean age were 26.11±2.61 for male, and 25.75±1.58 for female. There were no significant difference between male and female in age, SE refractive error, IOP, axial length, central corneal thickness, anterior chamber depth, lens thickness, pupil diameter, central subfield thickness, cube volume, and cube average thickness.
Table 3 shows the mean value of DVA at baseline, 1 week, and 4 weeks. In both gender, there were significant differences between monocular DVA and binocular DVA. Binocular DVA was significantly higher than monocular DVA (P < 0.01). But there was no significant differences between right DVA and left DVA. In comparison by gender, average right, left, and binocular DVA of men were significantly higher than those of women (P < 0.01).
Table 4 shows the mean value of KVA at baseline, 1 week, and 4 weeks. Similar to DVA, average right, left, and binocular KVA of men were higher than those of women (P < 0.01). However, no significant difference was noted between the monocular KVA and binocular KVA.
Table 5 and 6 show the pearson’s correlation between clinical or ocular factors and DVA and KVA, respectively. In men, DVA was associated with SE refractive error (r = −0.239, P = 0.039), axial length (r = −0.025, P = 0.033) and pupil diameter (r = 0.213, P = 0.048) and KVA was associated with SE refractive error (r = −0.227, P = 0.034), axial length (r = −0.016, P = 0.018). In women, DVA was associated with SE refractive error (r = −0.224, P = 0.041), axial length (r = −0.031, P = 0.049) and pupil diameter (r = 0.227, P = 0.041) and KVA was associated with SE refractive error (r = −0.204, P = 0.024), axial length (r = −0.029, P = 0.039).
This study shows that DVA and KVA are related to the several clinical and ocular factors, and men have better DVA and KVA than women. Compared to women, men are likely to spend more time for sports activity, this seems to be a reason that men have better DVA and KVA. To our knowledge, this is the first study investigating in domestic about DVA and KVA with ocular factors measured by optical low coherence reflectometry. Results of this study showed that SE refractive error and axial length could affect DVA and KVA, and pupil diameter could affect the DVA. Many studies[1-5] investigating DVA and KVA of various athletes have been reported but there never been studies considered ocular factors to the DVA and KVA.
Myopia is common ocular condition and continue to increases in prevalence, particularly in Asian populations.[16-19] As subjects had higher myopia and longer axial length, they showed worse DVA and KVA. Because more-myopic eyes tend to have lower SE refractive error and longer axial length, our results suggest that myopia might have negative correlation with DVA and KVA.[19]
DVA is typically tested by asking subjects to judge or identify dynamic objects while their head is fixed. This involves reporting the location of a small opening in a moving Landolt-C ring. This examines the ability of minimum resolvable capacity, which means the ability to discriminate two small shapes in space. Combination of different types of eye and head movements enables to stabilize the image of subject close to the fovea, the small area on retina where photoreceptor density and visual acuity are maximal.[ 20,21] Smooth pursuit eye movements aim to match the speed of gaze with that of small, moving visual targets, and can be used to track objects travelling at speeds of up to 50 degrees of visual angle per second. At higher target speeds, when gaze lags behind the target, the eyes use fast catch-up saccades to compensate for position and velocity errors.[22] In this study, pupil diameter had positive correlation with DVA in men and women, and it was statistically significant. However, it is unclear which mechanism lead pupil diameter to such DVA advantages. Further studies of relationship among the pupil size, smooth pursuit eye movements, and DVA would be needed.
There are several limitations of this study. First, we didn’t include athletic ability parameters of subjects. Some studies reported differences in DVA or KVA among the groups of different performance levels.[5,23] But Hoshina K et al reported there were no significant differences in DVA or KVA among the player groups.[24] Cumulated performance data were available for professional athletes but there was no data and no standard method to evaluate athletic performance of normal subjects. Further study will be needed to investigate standardized method evaluating athletic performance when measuring DVA or KVA. Another limitation of this study was that we measured DVA with the target moving from only right to left. Because effective eye movements are related to DVA, measuring DVA with moving targets of various directions such as left to right, superior to inferior, inferior to superior could be helpful for further studies.[25,26]
CONCLUSIONS
We investigated the characteristics of DVA and KVA in young myopic eyes and found that both DVA and KVA were significantly different between men and women, and showed that men had better DVA and KVA than women. Also, DVA and KVA can be measured significantly different by degree of myopia, axial length, pupil diameter. The lower degree of myopia, shorter axial length, and longer pupil diameter were associated with the higher DVA. Similarly, the lower degree of myopia and shorter axial length were associated with high KVA. However, KVA did not show association with pupil diameter. When measuring DVA and KVA, clinical factors, such as myopia and ocular biometry should be considered.
References
-
Ludvigh, E, The visibility of moving objects, Science, (1948), 108(2794), p63-64.
[https://doi.org/10.1126/science.108.2794.63]

- Miller, JW, Ludvigh, E, effect of relative motion on visual acuity, Surv Ophthalmol, (1962), 7, p83-116.
- Suzumura, A, Studies on the kinetic visual acuity especially on accommodation to the moving object: on the trial manufactured kinetic vision tester, model A.S. 3, Nippon Ganka Gakkai Zasshi, (1964), 68(10), p1277-1288.
- Laby, DM, Rosenbaum, AL, Kirschen, DG, Davidson, JL, Rosenbaum, LJ, Strasser, C, et al. , The visual function of professional baseball players, Am J Ophthalmol, (1996), 122(4), p476-485.
- Morris, GS, Kreighbaum, E, Dynamic visual acuity of varsity women volleyball and basketball players, Res Q, (1977), 48(2), p480-483.
- Winograd, S, The relationship of timing and vision to baseball performance, Res Q, (1942), 13(4), p481-483.
- Rouse, MW, DeLand, P, Christian, R, Hawley, J, A comparison study of dynamic visual acuity between athletes and nonathletes, J Am Optom Assoc, (1988), 59(12), p946-950.
-
Akman, A, Asena, L, Güngör, SG, Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500, Br J Ophthalmol, (2016), 100(9), p1201-1205.
[https://doi.org/10.1136/bjophthalmol-2015-307779]

-
McAlinden, C, Wang, Q, Gao, R, et al. , Axial length measurement failure rates with biometers using swept-source optical coherence tomography compared to partial-coherence interferometry and optical low-coherence interferometry, Am J Ophthalmol, (2017), 173, p64-69.
[https://doi.org/10.1016/j.ajo.2016.09.019]

-
Buckhurst, PJ, Wolffsohn, JS, Shah, S, Naroo, SA, Davies, LN, Berrow, EJ, A new optical low coherence reflectometry device for ocular biometry in cataract patients, J Ophthalmol, (2009), 93(7), p949-953.
[https://doi.org/10.1136/bjo.2008.156554]

-
Hoffer, KJ, Shammas, HJ, Savini, G, Comparison of 2 laser instruments for measuring axial length, J Cataract Refract Surg, (2010), 36(4), p644-648.
[https://doi.org/10.1016/j.jcrs.2009.11.007]

-
Bjeloš Rončević, M, Bušić, M, Cima, I, Kuzmanović Elabjer, B, Bosnar, D, Miletić, D, Intraobserver and interobserver repeatability of ocular components measurement in cataract eyes using a new optical low coherence reflectometer, Graefes Arch Clin Exp Ophthalmol, (2011), 249(1), p83-87.
[https://doi.org/10.1007/s00417-010-1546-z]

-
Shammas, HJ, Hoffer, KJ, Repeatability and reproducibility of biometry and keratometry measurements using a noncontact optical low-coherence reflectometer and keratometer, Am J Ophthalmol, (2012), 153(1), p55-61.
[https://doi.org/10.1016/j.ajo.2011.06.012]

-
Shim, HS, Kim, SH, Kang, HS, Changes in KVA resulting from correction condition of refractive error, J Korean Ophthalmic Opt Soc, (2013), 18(2), p165-171.
[https://doi.org/10.14479/jkoos.2013.18.2.165]

- Shim, MS, Kim, SH, Kang, HS, Shim, HS, The study of kinetic visual acuity in college students, J Korean Ophthalmic Opt Soc, (2012), 17(4), p419-424.
-
Sperduto, RD, Seigel, D, Roberts, J, Rowland, M, Prevalence of myopia in the United States, Arch Ophthalmol, (1983), 101(3), p405-407.
[https://doi.org/10.1001/archopht.1983.01040010405011]

- Wong, TY, Foster, PJ, Hee, J, Ng, TP, Tielsch, JM, Chew, SJ, Prevalence and risk factors for refractive errors in adult Chinese in Singapore, Invest Ophthalmol Vis Sci, (2000), 41(9), p2486-2494.
- Sawada, A, Tomidokoro, A, Araie, M, Iwase, A, Yamamoto, T, Refractive errors in an elderly Japanese population: the Tajimi study, Ophthalmology, (2008), 115(2), p363-370.
- Mc Brien, NA, Gentle, A, Role of the sclera in the development and pathological complications of myopia, Prog Retin Eye Res, (2003), 22(3), p307-338.
-
Jacobs, RJ, Visual resolution and contour interaction in the fovea and periphery, Vision Res, (1979), 19(11), p1187-1195.
[https://doi.org/10.1016/0042-6989(79)90183-4]

-
Hirsch, J, Curcio, CA, The spatial resolution capacity of human foveal retina, Vision Res, (1989), 29(9), p1095-1101.
[https://doi.org/10.1016/0042-6989(89)90058-8]

-
de Brouwer, S, Yuksel, D, Blohm, G, Missal, M, Lefèvre, P, What triggers catch-up saccades during visual tracking?, J Neurophysiol, (2002), 87(3), p1646-1650.
[https://doi.org/10.1152/jn.00432.2001]

- Stine, CD, Arterburn MR, Stern NS. Vision and sports: a review of the literature, J Am Optom Assoc, (1982), 53(8), p627-633.
- Hoshina, K, Tagami, Y, Mimura, O, Edagawa, H, Matsubara, M, Nakayama, T, A study of static, kinetic, and dynamic visual acuity in 102 Japanese professional baseball players, Clin Ophthalmol, (2013), 7, p627-632.
-
Barmack, NH, Dynamic visual acuity as an index of eye movement control, Vision Res, (1970), 10(12), p1377-1391.
[https://doi.org/10.1016/0042-6989(70)90089-1]

-
Brown, B, Dynamic visual acuity, eye movements and peripheral acuity for moving targets, Vision Res, (1972), 12(2), p305-321.
[https://doi.org/10.1016/0042-6989(72)90120-4]