Changes in Macular Pigment Optical Density and Visual Acuity after Lutein Supplementation in Adults in Their 20s

Abstract
This study was conducted to determine whether lutein supplementation (including zeaxanthin) improves macular pigment optical density (MPOD) and visual acuity.
One hundred and twenty adults in their 20s (60 subjects in the experimental group that received lutein, 60 subjects in the control group) who had no systemic diseases or specific eye diseases (macular pigment degeneration and cataract) were included and allocated to experimental and control groups. The experimental and control groups were administered with 20 mg lutein (which naturally contains 1.5 mg zeaxanthin) and soybean oil in pill form, respectively, once a day for 6 months. MPOD was measured with a Macular Pigment Screener II (MPS II ®) every month, while distance and near visual acuities, refractive error (S.E), and contrast sensitivity were measured before and after 6 months of the supplementation.
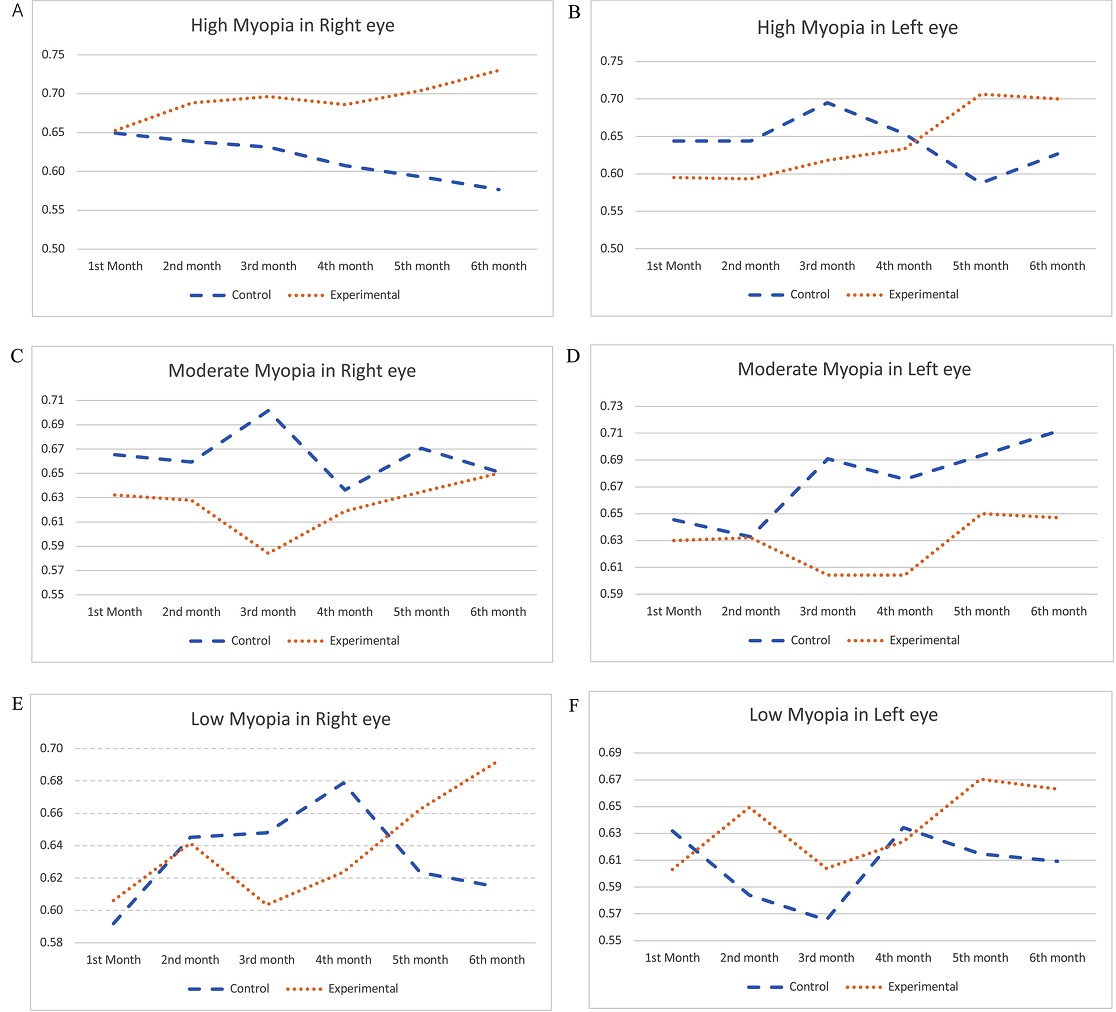
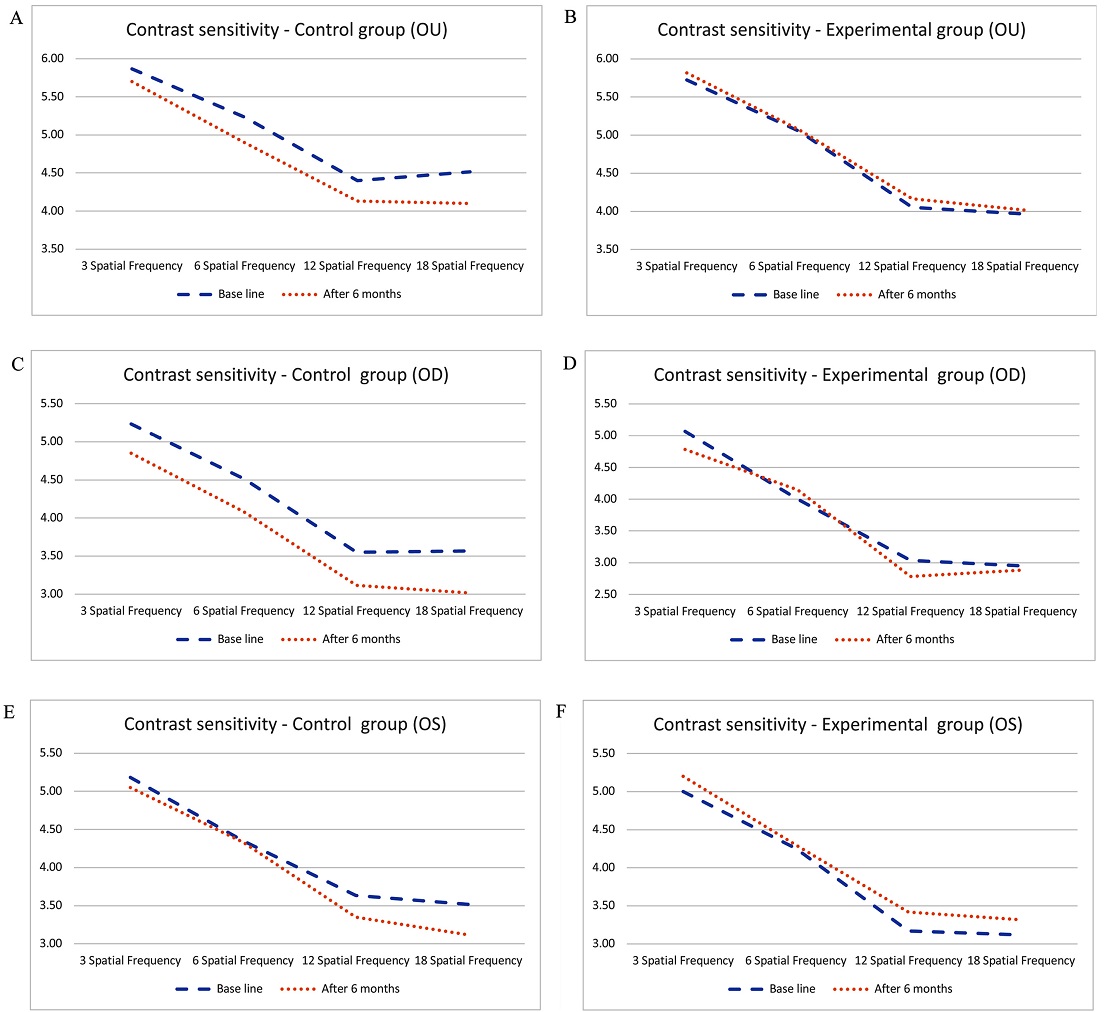
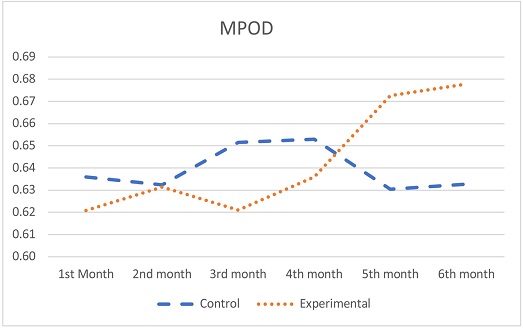
The MPOD in the control group did not improve after 6 months (baseline 0.64±0.10 to study end 0.63±0.13) in both eyes; the experimental group showed a statistically significant improvement from 0.62±0.11 before to 0.68±0.12 after the 6 months of supplementation (p=0.000, t=4.554). Subjects with high or low myopia in the experimental group also showed a statistically significant improvement in MPOD (right eye: high degree [p=0.029, t=2.435], low degree [p=0.000, t=4.160]; left eye: high degree [p=0.014, t=2.810], low degree [p=0.041, t=2.177]), while those with moderate myopia in the same group showed no significant change (right eye: p>0.05, t=0.569; left eye: p>0.05, t=0.535). The near visual acuities for both eyes in the experimental group significantly improved after the supplementation (p=0.001, t=3.419). Contrast sensitivity at most frequencies also improved for the right eye, left eye, and both eyes; there was no significant improvement in the right eye in the experimental group at high frequencies, and a decline was observed for all the frequencies in the right eye, left eye, and both eyes in the control group.
Lutein supplementation for 6 months improves MPOD, myopia, near visual acuity, and contrast sensitivity at selected frequencies.
초록
20대 성인에서 루테인(지아잔틴 포함) 섭취가 황반색소광학밀도(macular pigment optical density; MPOD)향상과 시각기능 개선에 영향이 있는지 알아보고자 하였다.
전신질환이나 특별한 안질환(황반색소변성 및 백내장)이 없는 20대 성인 120명(실험군 60명, 대조군 60명)을 대상으로 실시하였다. 실험군은 루테인을 대조군은 대조식품인 대두유를 동일한 알약형태로 6개월간 1일 1회씩 섭취하였다. 각각의 식품을 섭취한 후 MPOD를 Macular Pigment Screener II(MPS II ®)를 이용하여 매월 측정하였으며, 원거리와 근거리 나안시력, 굴절이상량(S.E), 그리고 대비감도 시력은 각각의 식품 섭취 전과 6개월 섭취 후에 측정하여 결과를 비교해 보았다.
대조군의 경우 대조식품 섭취 전 양안 MPOD는 0.64±0.10이었고 6개월 섭취 후는 0.63±0.13으로 감소한 반면, 실험군의 경우 루테인 섭취 전 양안 MPOD는 0.62±0.11이었고 6개월 섭취 후는 0.68±0.12로 루테인을 섭취한 실험군의 MPOD가 통계적으로 유의하게 증가하였다(p=0.000, t=4.554). 근시 정도별로는 고도, 약도 근시는 루테인을 섭취한 실험군이 통계적으로 유의하게 향상한 것으로 나타났으나(우안: 고도 p=0.029, t=2.435, 약도 p=0.000, t=4.160 / 좌안: 고도 p=0.014, t=2.810, 약도 p=0.041, t=2.177), 중도 근시에서는 유의하지 않았다(우안: p>0.05, t=0.569, 좌안: p>0.05, t=0.535). 근거리 양안 나안시력은 루테인을 섭취한 실험군에서 섭취 전과 비교하여 통계적으로 유의하게 향상된 것으로 나타났다(p=0.001, t=3.419). 대비감도 시력은 루테인을 섭취한 실험군의 경우 우안 고주파수대 일부를 제외하고 우안, 좌안, 양안 대부분의 주파수에서 향상되는 것으로 나타났으나, 대조군의 경우 우안, 좌안, 양안 모든 주파수에서 감소하는 경향이 나타났다.
이러한 결과로 볼 때, 6개월간의 루테인 섭취가 황반색소광학밀도(MPOD) 향상에 효과가 있었으며, 근시정도, 근거리 나안시력, 일부 대비감도 시력 등의 시각기능이 향상되는 것을 알 수 있었다.
Keywords:
Macular pigment optical density, Lutein, Zeaxanthin, Contrast sensitivity키워드:
황반색소광학밀도, 루테인, 지아잔틴, 대비감도시력Introduction
There is a spot called macula in the retina of our eyes. The nerve tissue located in this center of the retina plays a crucial role in our ability to see objects. Since it is where visual cells are concentrated most and images are formed, it is not too much to say that the health of macula determines the eyesight. It is known that the center of the macula consists of a substance called zeaxanthin and the periphery consists of lutein.
Lutein is a carotenoid with strong antioxidant activity and is absorbing blue light. Lutein is found in high quantities in green and yellow vegetables such as spinach, green bean, and broccoli.[1] Lutein and zeaxanthin in the vegetables or supplements are reported to help protect eyes from exposure to blue light in primates and human adults.[2,3] They do so by absorbing blue light and by acting as a filter that reduces the photochemistry damage by high energy blue light in the retina and are reported to act as an antioxidant that prevents the oxidative damage of retina by the harmful light.[4,5] Although there has been no data on the influence of supplements such as lutein on the eyesight of children, some studies showed that they are beneficial for adult patients with visual function problems, like Age Related Macular Degeneration.[6,7] As reported from the studies above, lutein and zeaxanthin can only be obtained from food such as green and yellow vegetables or supplements because they are not synthesized in the human body.[8] The substances are also getting more attention in other fields then eye health, as a recent study suggested their influence on skin health[9] and brain health.[10] Researchers including Hammond BR published studies on the effects of lutein on macular pigment optical density (MPOD).[11] In Korea, related studies have mainly focused on health impact assessment, [12] health functional food recognition,[13] substance extraction condition,[14] and eye health care,[15] and there has been hardly any studies on the direct effects on eyes.
According to the Korea National Health Statistics in 2012, the animal-based food consumption has been on the rise from below 10% in the mid-1970s to above 20% in the 1990s and reached 20.6% in 2012 whereas the plant-based food consumption has decreased.[16] As the statistics suggest, Koreans in their 20s have very low consumption levels of green and yellow vegetables as the diets have been westernized. By that, less lutein is consumed by vegetables which leads to a less dense macular pigment. On the other side, the younger generation is much more exposed to blue light due to usage of digital devices including smartphones or in-house lightening by LEDs. Therefore, this study was conducted to investigate of lutein supplementation has a beneficial impact on MPOD and on visual functions in Koreans.
Subject and Method
1. Subject
This study was conducted on 120 adults (60 subjects in the experimental group, 60 subjects in the control group) without any systemic diseases or particular eye diseases (macular pigment degeneration and cataract) who understood the contents and agreed to participate.
2. Supplementation Contents and Method
The experimental group received a dietary supplement containing lutein and zeaxanthin in the ratio of 20 mg : 1.5 mg in pill form (hereinafter referred to lutein) once a day. The 1.5 mg zeaxanthin is naturally present in the lutein powder.
The control group received a pill containing soybean oil (hereinafter referred to control food) once a day.
The study participants took either lutein (test food) or the control food once a day for 6 months from June 2019 to November 2019.
This study was a double-blind study. This setup prevents that neither the researches nor the study participants know in which intervention group (experimental group or control) the study participant was.
3. Test Method
Basic information on the subjects was collected, which included the presence of systemic diseases or eye diseases, history of eye surgery, medication, and vision correction method.
Using a macular pigment screener II (MPS II ®; Elektron Eye Technology, Cambridge, UK, Klarity Inc. in Korea), macular pigment optical density (MPOD) was measured in both eyes in the experimental group once a month for 6 months and in the control group only at the beginning and the end of the 6 months intervention period.
The MPS II is a computerized device designed for measuring MPOD and used to identify patients at the risk for the early development of AMD.[16] The device measures the attenuation of blue light by macular pigments in density units (DU) in the range from 0 to 1. Heterochromatic flicker photometry (HFP) is used as the measurement method, and the background brightness is set at 250 cdm-2 to lower the impact on rod cells and cone cells including s-cones in particular. A researcher initiates the measurement with a noninvasive, low intensity light that does not require pupil dilation by pushing the start button when a subject is looking at the blinking light. The technique uses the property of macular pigment, which is to absorb the spectrum of lights ranged from blue to green (460 nm-570 nm). MPOD is determined during the process of alternating the lights which macular pigment are known to absorb at fovea centralis and periphery that the macular pigment and adjusting the lights’ relative intensities until the sensation of flicker is minimized or disappeared. This is based on the assumption that macular pigment density is at its maximum at the fovea centralis, and it decreases exponentially at 6 to 8 degrees eccentricity to the minimum or zero. The measurements are given by log [MPOD = Log 10(Bf/Bp)], which represents the comparison between the light intensities needed at the center (Bf) and periphery (Bp).[18]
The examination room intensity of illumination was conducted about 200 lux. Because, Woo and Long mention that 800 to 1,000 lux of illumination on the vision chart and 130 to 215 lux around the vision chart were appropriate.[19] Using the Randolt ring in the distance vision chart for 5 meters (Hubitz HDC-9000), the distance visual acuity was measured individually on each eye of subjects in the experimental group before (the beginning of study) and after lutein supplementation (after 6 months). The same was performed on subjects in the control group with the supplementation of control food.
The examination room intensity of illumination was conducted about 200 lux. Because, Woo and Long mention that 800 to 1,000 lux of illumination on the vision chart and 130 to 215 lux around the vision chart were appropriate.[19]
Using the Randolt ring in the near vision chart for 40 cm (Hubitz near vision chart), the distance visual acuity was measured individually on each eye, of subjects in the experimental group before (the beginning of study) and after lutein supplementation (after 6 months). The same was performed on subjects in the control group with the supplementation of control food.
Using an objective auto-refractometer (NIDEK ARK-1A, Figure 2), the refraction was measured individually on each eye, of subjects in the experimental group before and after lutein supplementation (after 6 months). The same was performed on subjects in the control group with the supplementation of control food.
Using the distance contrast sensitivity chart (Vector Vision CSV-1000E, Figure 2), the contrast sensitivity was measured individually on each eye of subjects in the experimental group before and after lutein supplementation (after 6 months) under full correction. The same was performed on subjects in the control group with the supplementation of control food.
The distance contrast sensitivity chart is a contrast sensitivity chart with a striped pattern. The striped pattern has 3, 6, 12, 18 cycles/degree (cpd) with the spatial frequency increasing towards the bottom and the contrast sensitivity decreasing towards the right. The cpd unit represents the number of stripes per degree.
4. Statistics
Statistics was only done one the PP (per protocol) population. This is the group of people who took the supplements every day and completed all tests and thus were fully compliant with the study procedures described in the protocol.
Paired t-test in SPSS (25.0 ver) was used to identify the difference in distance and near visual acuity, contrast sensitivity, and MPOD between the experimental group and the control group, and test results were considered statistically significant when the significance level is less than 0.05.
Result and Discussion
1. Changes in MPOD in both eyes
The control group of 60 subjects consisted of 27 men and 33 women, and the experimental group of 60 subjects consisted of 35 men and 25 women. The average age was 22.8±2.66 in the control group and 23.35±2.71 in the experimental group (Table 1).
The control group showed a slight decrease in MPOD from 0.64±0.10 before the supplementation of control food and 0.63±0.13 after the 6 months supplementation. On the other hand, the experimental lutein group showed a statistically significant increase by about 0.06 in MPOD from 0.62±0.11 before the supplementation of lutein and 0.68±0.12 after the supplementation. The difference between the MPOD results in both eyes before and after the supplementation was higher in the experimental group, which was also statistically significant (p=0.000, t=4.554) (Table 2 & Fig. 3). Preceding studies, including one by Hammond, demonstrated that the 6 months of lutein supplementation increased MPOD by about 0.05, as also shown in this study, and reported a significant increase in MPOD in the areas 10, 30, 60, and 105 minutes away from the fovea centralis in the experimental group supplemented with lutein 10 mg and zeaxanthin 2 mg for 1 year when compared to a control group. Also, the experimental lutein group showed a significant improvement in contrast sensitivity as well as recovery time from light stress.[11] Many preceding studies, including ons by Stringham and Hammond, have reported that the experimental group supplemented with lutein and zeaxanthin showed improvement in MPOD.[20-26]

Comparison between macular pigment optical densities of the experimental and control groups after 6 months
Significant increase in macular pigment optical density in the experimental group compared to the control group.
In addition, the significant improvement of MPOD was seen in both genders, when comparing the genders in the control and the experimental group (p=0.005 in men, p=0.001 in women, Table 3).
2. Changes in MPOD according to the degree of myopia with refractive errors
The spherical equivalent was calculated to determine the degree of refractive error. Efron[27] classified the progression of myopia into three degrees: low degree (0.00 ~ −2.75 D), moderate degree (−3.00~−5.00 D), and high degree (<−5.00 D). This study also measured the changes in MPOD in the right and left eyes according to each degree of myopia in the control group and the experimental group.
In the right eye, subjects with high degree myopia in the control group showed a decrease in MPOD from 0.65±0.12 before the supplementation to 0.58±0.17 after 6 months of the control supplementation while those in the experimental lutein group showed a statistically significant increase from 0.65±0.13 before the supplementation to 0.73±0.12 after 6 months (p=0.029, t=2.435).
Subjects with moderate degree myopia in the control group showed a decrease in MPOD in the right eye from 0.67±0.10 before the supplementation to 0.65±0.14 after 6 months of the supplementation while those in the experimental group showed an increase from 0.65±0.15 before the supplementation of lutein to 0.63±0.14 after 6 months, however without a statistically significant difference (p>0.05, t=0.569).
Subjects with low degree myopia in the control group showed a slight increase in MPOD in the right eye from 0.59±0.11 before the supplementation to 0.61±0.16 after 6 months of the supplementation while those in the experimental group showed a statistically significant increase from 0.61±0.08 before the supplementation to 0.69±0.11 after 6 months after the supplementation (p=0.000, t= 4.160) (Table 4, Table 5 & Fig. 4).
In the left eye, subjects with high degree myopia in the control group showed a decrease in MPOD from 0.64±0.16 before the supplementation of control food to 0.63±0.14 after 6 months of the supplementation while those in the experimental group, unlike the control group, showed a statistically significant increase from 0.60±0.14 before the supplementation of lutein to 0.70±0.09 after 6 months after the supplementation (p=0.014, t=2.810).
Subjects with moderate degree myopia in the control group and the experimental group both showed an increase in MPOD in the left eye from 0.65±0.09 to 0.71±0.14 and from 0.63±0.15 to 0.65±0.16 before and after the supplementation. However, there was no significant difference (p=0.598, t=0.535).
Subjects with low degree myopia in the control group showed a decrease in MPOD from 0.63±0.09 before the supplementation to 0.62±0.14 after 6 months of the supplementation while those in the experimental group showed a statistically significant increase from 0.60±0.13 before the supplementation to 0.66±0.08 after 6 months after the supplementation (p=0.041, t = 2.177) (Table 4, Table 5 & Fig. 4).
3. Changes in distance visual acuity
The control group showed a slight decrease in the distance visual acuity in both eyes from 0.54±0.52 before the supplementation to 0.53±0.53 after 6 months of the supplementation while the experimental lutein group showed no statistically significant difference from 0.41±0.50 before the supplementation to 0.41±0.47 after the supplementation (p>0.005, t=−0.219) (Table 5). Unlike this study, however, a study conducted by Piermarocchi has reported that the group supplemented with lutein 10 mg and zeaxanthin 1 mg for 2 years showed improvement in the visual acuity.[28] Thus, the insignificant change of visual acuity in this study is considered to be derived from the short period of supplementation, which lasted only for 6 months, and further studies with a longer period of time are considered to be needed.
4. Changes in near visual acuity
The near visual acuity in the control group was 0.57±0.39 before the supplementation of control food and 0.61±0.40 after the supplementation, and that in the experimental lutein group was improved from 0.47±0.38 before the take of lutein to 0.55±0.40 after the supplementation with a statistically significant difference (p=0.001, t=3.419, Table 6).

Comparison between distance visual acuities of the control and the; experimental groups after 6 months
5. Changes in contrast sensitivity and MPOD
In case of the contrast sensitivity (at 3 / 6 / 12 / 18 cpd) in both eyes, the control group showed a decrease from 5.87 / 5.23 / 4.40 / 4.52 before the supplementation to 5.70 / 4.90 / 4.13 / 4.10 after 6 months of supplementation while the experimental group showed 5.72 / 5.05 / 4.05/ 3.97 before the supplementation of lutein and 5.82 / 5.07 / 4.17 / 4.02 after 6 months of the supplementation. The contrast sensitivity comparison between before and after the supplementation in the control group and the experimental group showed no statistically significant difference with p>0.05 (Table 8, Table 9). However, as suggested in Figure 5 and Table 1, the control group showed decreasing trends at all cpd in the right eye, the left eye, and the both eyes while the experimental group showed improvement at all cpd expect the high frequency in the right eye when before and after the supplementation were compared. Studies including one by Yao reported that the supplementation of lutein 20 mg for 1 year improved the contrast sensitivity with a statistically significant difference although the improvement in the corrected vision showed no statistically significant difference.[29] Also, studies including one by Ma reported that the group supplemented with lutein 20 mg for 48 weeks showed improvement in the contrast sensitivity.[30] The differences between this study and preceding studies are considered to be derived from the short period of supplementation and further studies with a longer period of time are considered to be needed.
Conclusion
Since Koreans in their 20s have very low consumption levels of green and yellow vegetables as their diets have been westernized and as this age group is over-exposed to blue light almost all day from digital devices including smartphones or in-house lightening from LEDs, the conditions are expected to influence their eye sight impacted by reduced MPOD levels. This study was conducted for this reason.
This study investigated the MPOD of 60 subjects in the control group and 60 subjects in an experimental lutein group. The control group showed almost no change in MPOD in both eyes between before and after the supplementation while the experimental lutein group showed a statistically significant increase in the same measurements. The MPOD according to the degree of myopia also showed greater improvement in subjects with high and low myopia in the experimental group when compared to the control group. Middle myopia showed slightly improvement. but, were not statistically significant. Preceding studies have shown that intake of lutein & zeaxanthin for 1 to 2 years resulted in significant changes. Therefore, it is assumed that further research is needed.
In addition, the experimental group showed a statistically significant increase in the near visual acuity and greater improvement in the contrast sensitivity than the control group when the measurements between before and after the supplementation were compared. Although not statistically significant, the control group was a slight decrease in distance visual acuity after six months, while the experimental lutein group was neither increase nor decrease in distance visual acuity. This shows that taking lutein and zeaxanthin has a fine effect on vision. Therefore, further research is needed. Even in the same subject's eyes, the right eye and the left eye's corrective vision will be different. When lutein & zeaxanthin were taken, the reactions in the right eye and left eye were measured slightly differently.
Preceding studies have shown that lutein increased MPOD and the speed was significantly faster in the experimental group supplemented with lutein than the control group. It is also reported that the change rate of MPOD was higher as the starting MPOD was lower in the experimental group.[31] In a study conducted by Hammond, the experimental group supplemented with lutein 10 mg and zeaxanthin 2 mg for 1 year showed a significant increase in MPOD, contrast sensitivity, and recovery speed from light stress.[11]
These studies demonstrated that the supplementation of lutein and zeaxanthin relieves the damage of retina caused by light oxidative stress by absorbing blue light. The mechanism was proven to improve the contrast sensitivity and relieve the light stress, which are functions of fovea centralis.
The result of this study also showed that the 6-month supplementation of lutein 20 mg and zeaxanthin 1.5 mg in Koreans in their 20s improved the MPOD, degree of myopia, near visual acuity, and some contrast sensitivities.
Acknowledgments
We are grateful for support from DSM Nutritional Products Ltd,. DSM provided Flora GLO Lutein 20 percent SAF products for using samples in this study. We also would like to express our gratitude for their useful comments to Ahngook health., Ltd
References
-
Hammond BR, Wooten BR, Curran-Celentano J. Carotenoids in the retina and lens: possible acute and chronic effects on human visual performance. Arch Biochem Biophys. 2001;385(1):41-46.
[https://doi.org/10.1006/abbi.2000.2184]

-
Landrum JT, Bone RA. Lutein, zeaxanthin, and the macular pigment. Arch Biochem Biophys. 2001;385(1):28-40.
[https://doi.org/10.1006/abbi.2000.2171]

- Zimmer JP, Hammond BR Jr. Possible influences of lutein and zeaxanthin on the developing retina. Clin Ophthalmol. 2007;1(1):25-35.
-
Krinsky NI, Landrum JT, Bone RA. Biologic mechanisms of the protective role of lutein and zeaxanthin in the eye. Annu Rev Nutr. 2003;23:171-201.
[https://doi.org/10.1146/annurev.nutr.23.011702.073307]

-
Krinsky NI, Johnson EJ. Carotenoid actions and their relation to health and disease. Mol Aspects Med. 2005;26(6):459-516.
[https://doi.org/10.1016/j.mam.2005.10.001]

- Bahrami H, Melia M, Yang L, et al. The effect of lutein supplementation in preservation of visual function in retinitis pigmentosa; a randomized double-blind placebo-controlled clinical trial. Invest Ophthalmol Vis Sci. 2004;45(13):5161.
- Dagnelie G, Zorge IS, McDonald TM. Lutein improves visual function in some patients with retinal degeneration: a pilot study via the Internet. Optometry. 2000;71(3):147-164.
-
Loane E, Nolan JM, O'Donovan O, et al. Transport and retinal capture of lutein and zeaxanthin with reference to age-related macular degeneration. Surv Ophthalmol. 2008;53(1):68-81.
[https://doi.org/10.1016/j.survophthal.2007.10.008]

-
Roberts RL, Green J, Lewis B. Lutein and zeaxanthin in eye and skin health. Clin Dermatol. 2009;27(2):195-201.
[https://doi.org/10.1016/j.clindermatol.2008.01.011]

-
Bovier ER, Renzi LM, Hammond BR. A double-blind, placebo-controlled study on the effects of lutein and zeaxanthin on neural processing speed and efficiency. PLos ONE. 2014;9(9):e108178.
[https://doi.org/10.1371/journal.pone.0108178]

-
Hammond BR, Fletcher LM, Roos F, et al. A doubleblind, placebo-controlled study on the effects of lutein and zeaxanthin on photostress recovery, glare disability, and chromatic contrast. Invest Ophthalmol Vis Sci. 2014;55(12):8583-8589.
[https://doi.org/10.1167/iovs.14-15573]

-
Lee EK, Choi JH, Heo YR. Intake of fruits and vegetables may modify the risk of cataract in Korean males: data from Korean National Health and Nutrition Examination Survey 2012. J Nutr Health. 2018;51(5):423-432.
[https://doi.org/10.4163/jnh.2018.51.5.423]

-
Kim YS, Choi BB. Recognition and consumption for the health functional food of college students in the northern Gyeonggi-do area. Korean J Food Nutr. 2016;29(2):206-217.
[https://doi.org/10.9799/ksfan.2016.29.2.206]

- Li M, Jang GY, Lee SH, et al. Lutein, β-carotene, and polyphenol contents of sweet potato leaves under different extraction conditions. Korean J Food Nutr. 2017;46(11):1343-1349.
-
Sim JG, Ye KH, Kwon OH, et al. An analysis on the quality of hand-washing and practice related to eye health care of adults. J Korean Ophthalmic Opt Soc. 2018;23(3):173-180.
[https://doi.org/10.14479/jkoos.2018.23.3.173]

- Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012 : Korea National Health and Nutrition Examination Survey (KNHANESV-3). Cheongwon : Korea Centers for Disease Control and Prevention ; 2013. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3937975/
-
Stringham JM, Hammond BR. The glare hypothesis of macular pigment function. Optom Vis Sci. 2007;84(9):859-864.
[https://doi.org/10.1097/OPX.0b013e3181559c2b]

- Wooten BR, Hammond BR, Land RI, et al. A practical method for measuring macular pigment optical density. Invest Ophthalmol Vis Sci. 1999;40(11):2481-2489.
- Woo GCS, Long WF. Recommended light levels for clinical procedures. Optom Monthly. 1979;70:720-725.
-
Stringham JM, Hammond BR. Macular pigment and visual performance under glare conditions. Optom Vis Sci. 2008;85(2):82-88.
[https://doi.org/10.1097/OPX.0b013e318162266e]

-
Richer S, Stiles W, Statkute L, et al. Double-masked, placebo-controlled, randomized trial of lutein and antioxidant supplementation in the intervention of atrophic age-related macular degeneration: The Veterans LAST study (Lutein Antioxidant Supplementation Trial). Optometry. 2004;75(4):216-229.
[https://doi.org/10.1016/S1529-1839(04)70049-4]

-
Weigert G, Kaya S, Pemp B, et al. Effects of lutein supplementation on macular pigment optical density and visual acuity in patients with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52(11):8174-8178.
[https://doi.org/10.1167/iovs.11-7522]

-
Murray IJ, Makridaki M, van der Veen RLP, et al. Lutein supplementation over a one-year period in early AMD might have a mild beneficial effect on visual acuity: The CLEAR study. Invest Ophthalmol Vis Sci. 2013;54(3):1781-1788.
[https://doi.org/10.1167/iovs.12-10715]

-
Wang X, Jiang C, Zhang Y, et al. Role of lutein supplementation in the management of age-related macular degeneration: meta-analysis of randomized controlled trials. Ophthalmic Res. 2014;52(4):198-205.
[https://doi.org/10.1159/000363327]

-
Stringham JM, Stringham NT. Serum and retinal responses to three different doses of macular carotenoids over 12 weeks of supplementation. Exp Eye Res. 2016;151:1-8.
[https://doi.org/10.1016/j.exer.2016.07.005]

-
Bone RA, Landrum JT. Dose-dependent response of serum lutein and macular pigment optical density to supplementation with lutein esters. Arch Biochem Biophys. 2010;504(1):50-55.
[https://doi.org/10.1016/j.abb.2010.06.019]

- Efron N. Optometry A-Z Hardcover, 1st Ed. London: Butterworth-Heinemann, 2006;227.
-
Piermarocchi S, Saviano S, Parisi V, et al. Carotenoids in Age-related Maculopathy Italian Study (CARMIS): twoyear results of a randomized study. Eur J Ophthalmol. 2012;22(2):216-225.
[https://doi.org/10.5301/ejo.5000069]

-
Yao Y, Qiu Q, Wu XW, et al. Lutein supplementation improves visual performance in Chinese drivers: 1-year randomized, double-blind, placebo-controlled study. Nutrition. 2013;29(7-8):958-964.
[https://doi.org/10.1016/j.nut.2012.10.017]

-
Ma L, Yan SF, Huang YM, et al. Effect of lutein and zeaxanthin on macular pigment and visual function in patients with early age-related macular degeneration. Ophthalmology. 2012;119(11):2290-2297.
[https://doi.org/10.1016/j.ophtha.2012.06.014]

-
Richer S, Devenport J, Lang JC. Differential temporal responses of macular pigment optical density in patients with atrophic age-related macular degeneration to dietary supplementation with xanthophylls. Optometry. 2007;78(5):213-219.
[https://doi.org/10.1016/j.optm.2006.10.019]