Factors Affecting Contrast Sensitivity Function in Refractive Surgery Patients



Abstract
To analyze the factors influencing contrast sensitivity function to evaluate visual quality after corneal refractive surgery.
Fifty-four subjects (age, 23.56±2.38 years) who underwent conventional laser in situ keratomileusis were included. From the measured contrast sensitivity data, the area under the log contrast sensitivity function (AULCSF) was calculated. The contribution of all independent variables to AULCSF under photopic and mesopic lighting conditions after surgery was assessed using backward stepwise multiple regression analysis.
In the final multiple regression model, in order of influence, corrected spherical equivalent (p=0.021), uncorrected distance visual acuity (p=0.021), total higher-order aberrations (HOAs) (p=0.030), spherical aberration (p=0.045), and ablation depth (p=0.048) were significantly associated with the photopic AULCSF. In order of influence, objective scatter index (p<0.001), total HOAs (p=0.008), and scotopic pupil size (p=0.031), were significantly associated with the mesopic AULCSF.
The findings of this study suggest that ocular HOAs were a factor influencing contrast sensitivity regardless of the lighting conditions, and intraocular scattering had a much greater effect on mesopic contrast sensitivity than photopic contrast sensitivity in corneal refractive surgery patients.
초록
각막굴절교정수술 후 시력의 질을 평가하기 위해 대비감도함수에 영향을 미치는 요인을 분석하였다.
일반적인 라식수술을 받은 54명(23.56±2.38세)을 대상으로 하였고, 측정한 대비감도 데이터로부터 로그 대비감도함수 아래의 영역(AULCSF)을 계산하였다. 굴절수술 후 밝은 조명 상태와 어두운 조명 상태에서 AULCSF에 대한 모든 독립변수들의 기여도는 후진선택방법의 다중회귀분석을 사용하여 평가하였다.
최종 다중회귀모델에서, 밝은 조명 상태의 AULCSF에 유의하게 영향을 미치는 변수는 교정된 등가구면굴절력(p=0.021), 원거리나안시력(p=0.021), 전체고위수차(p=0.030), 구면수차(p=0.045), 각막절삭량(p=0.048)으로 나타났고, 어두운 조명 상태의 AULCSF에 유의하게 영향을 미치는 변수는 OSI(p<0.001), 전체고위수차(p=0.008), 암소시의 동공크기(p=0.031)로 나타났다.
본 연구의 결과는 각막굴절수술안에서 눈의 고위수차는 조명의 밝기에 상관없이 대비감도에 영향을 미치는 요인이며, 안구내 빛의 산란은 밝은 조명 상태의 대비감도보다 어두운 상태의 대비감도에 훨씬 더 큰 영향을 줄 수 있음을 시사한다.
Keywords:
Contrast sensitivity function, Refractive surgery, Visual quality키워드:
대비감도함수, 굴절수술, 시력의 질Introduction
Laser refractive surgery with the laser in situ keratomileusis(LASIK) surgical technique has been widely practiced to correct refractive error, especially in patients with myopia. Since myopic refractive surgery corrects refractive error by flattening the radius of curvature of the central cornea, this change in the corneal shape may affect the ocular optical system. Ocular aberrations and ocular scattering are known to result in degradation of retinal image quality in visual function.[1-3] Previous studies reported that the quality of vision after corneal refractive surgery deteriorated due to symptoms such as glare, light blur, and halos.[4-6] In particular, there has been interest in whether the preoperative refractive error has an effect on visual function in relation to the correction of high myopia and astigmatism.[7-8]
The contrast sensitivity function measures contrast sensitivity, representing visual sensitivity for a range of spatial frequencies and provides more characterizing visual information about how well the visual system performs in contrast to the visual acuity test with high-contrast black and white.[9,10] Contrast sensitivity testing has proven to be clinically useful in detecting visual impairments that are not detected by the usual visual acuity test.[11-14] Additionally, because contrast sensitivity tests measure sensitivity of the reduced contrast in a given spatial frequency range, it can more efficiently evaluate the quality of vision in an environment similar to the contrast encountered in daily life.[15,16] Accordingly, to effectively evaluate the visual performance after LASIK surgery, it is necessary to conduct visual function tests related to visual quality with various contrasts under different lighting conditions. The purpose of this study was to investigate the factors affecting the contrast sensitivity function under photopic and mesopic lighting conditions to assess visual quality in subjects who underwent conventional LASIK.
Subject and Methods
1. Subjects
In total, 108 eyes of the 54 subjects who underwent conventional myopic LASIK surgery, with no ocular diseases except for dry eye disease and who met the criterion (i.e., best unaided monocular visual acuity of 0.9 or better) were included in this study. Written informed consent was obtained from the subjects who participated in the study following a detailed explanation of the study procedures.
2. Measurement of Biometric Data
The natural mesopic and scotopic pupil sizes were measured using a digital variable pupillometer (VIPTM - 200, Neuroptics, USA) under dark conditions. Corneal thickness and corneal asphericity (Q-value) were measured using a rotating Scheimpflug imaging system (Pentacam HR, Oculus, Wetzlar, Germany). Data related to ablation depth and optical zone diameter were obtained from patients who underwent LASIK.
3. Assessment of Visual Acuity and Contrast Sensitivity Function
Uncorrected distance visual acuity (UCDVA) measurements were performed using a high contrast (100%) ETDRS acuity chart at a distance of 4 m. UCDVA was recorded using logMAR units. Additionally, the refractive error and K-readings were measured using an automated refractometer (KR-8100P, Topcon, Tokyo, Japan) and a phoropter (VT-SE, Topcon, Tokyo, Japan). The test was performed monocularly. The contrast sensitivity function was measured using a contrast sensitivity unit(CSV-1000E, Vector Vision, Dayton, USA) under photopic(340 lx) and mesopic (1 lx) lighting conditions to evaluate visual quality. At each testing session, contrast sensitivity was measured for four spatial frequencies (3, 6, 12, and 18 cycles/degree [cpd]) at 2.5 m. The testing was performed monocularly. From the data obtained with the CSV-1000E, the area under the log contrast sensitivity function (AULCSF) was calculated according to the method of Applegate et al,[17] according to whom the log of contrast sensitivity was plotted as a function of log spatial frequency, and third-order polynomials were fitted to the data. The fitted function was integrated between the fixed limits of log spatial frequencies of 0.48 (corresponding to 3 cpd) and 1.26 (corresponding to 18 cpd), and the resultant value was defined as the AULCSF.
4. Measurement of Ocular Aberrations and Ocular Scattering
Ocular aberrations were measured using a wavefront analyzer (KR-1W, Topcon, Tokyo, Japan) with the Hartmann-Shack (HS) technique. The HS sensor is the most commonly used wavefront sensor for evaluating the quality of retinal images.[18,19] Ocular aberrations analyzed included lower-order aberrations (LOAs) and higher-order aberrations (HOAs) in a 4-mm pupil. LOAs, the second-order aberrations, include spherical defocus and astigmatism. HOAs analyzed included total HOAs, comas were included in third-order aberrations, and spherical aberrations (SAs) were included in fourth-order aberrations. Ocular aberrations were calculated as root-mean-square(RMS) values. To maximize the influence of pupil size, ocular aberrations were measured under mesopic lighting conditions (1 lx).
Ocular optical quality parameters, which indicate the quality of retinal images, were obtained using an Optical Quality Analysis System (OQASII, Visiometrics, Terrassa, Spain) based on the double-pass technique, for a 4 mm pupil. Measurements using OQAS were conducted under mesopic conditions (1 lx) with an undilated pupil. The OQAS provides the objective scattering index (OSI), MTF cut-off, and Strehl ratio. The OSI, as a numerical value obtained by quantifying the degree of intraocular forward scattered light, is calculated by evaluating the amount of light outside the double-pass retinal intensity point spread function (PSF) image related to the amount of light in the center.[20,21] The OSI would range around 1.0 for a normal eye, and the larger the OSI value, the greater is the ocular scattering.[21] The Strehl ratio represents the ratio of the maximum focal intensity in the aberrated image that corresponds to the ideal PSF.[22] The Strehl ratio ranges from 0 to 1.0, with 1.0 indicating a perfect optical system with no aberrations, and the higher the Strehl ratio value, the better is the ocular optical quality. MTF represents the contrast loss produced by ocular optics as a function of spatial frequency, providing information about the overall ocular optical performance.[23] The MTF cutoff is the spatial frequency at which the 0.01 value of MTF is reached,[20] and the higher the MTF cut-off value, the better is the ocular optical quality.
5. Statistical Analyses
The contribution of all independent variables to AULCSF in LASIK subjects was assessed using multivariate regression analysis. AULCSF was used as the dependent variable. Independent variables included corneal thickness, optical zone diameter, ablation depth, corrected SE, UCDVA, mesopic and scotopic pupil sizes, Q-value, spherical defocus and astigmatism, total HOAs, coma and spherical aberration, OSI, MTF cut-off, and Strehl ratio. Multiple regression analysis was performed with backward stepwise removal method to select an appropriate model, and a p-value of more than 0.20 was used for removal. Durbin-Watson and variance inflation factors were used to avoid the problem of multicollinearity among the independent variables. The Pearson correlation test was used to determine the relationships among the independent variables in the LASIK subjects. All statistical analyses were conducted using SPSS version 21.0 (SPSS, Chicago, IL). The results were expressed as mean±standard deviation (SD), and a p-value of less than 0.05 was considered statistically significant.
Results
1. Characteristics of Subjects
The demographic and clinical data of the study participants are shown in Table 1. Fifty-four subjects (108 eyes) who underwent conventional myopic LASIK surgery participated in this study. The mean age of the subjects was 23.56±2.38 years. The mean UCDVA expressed as logMAR was −0.03±0.06 (−0.20 to 0.12).
2. Contrast Sensitivity Function
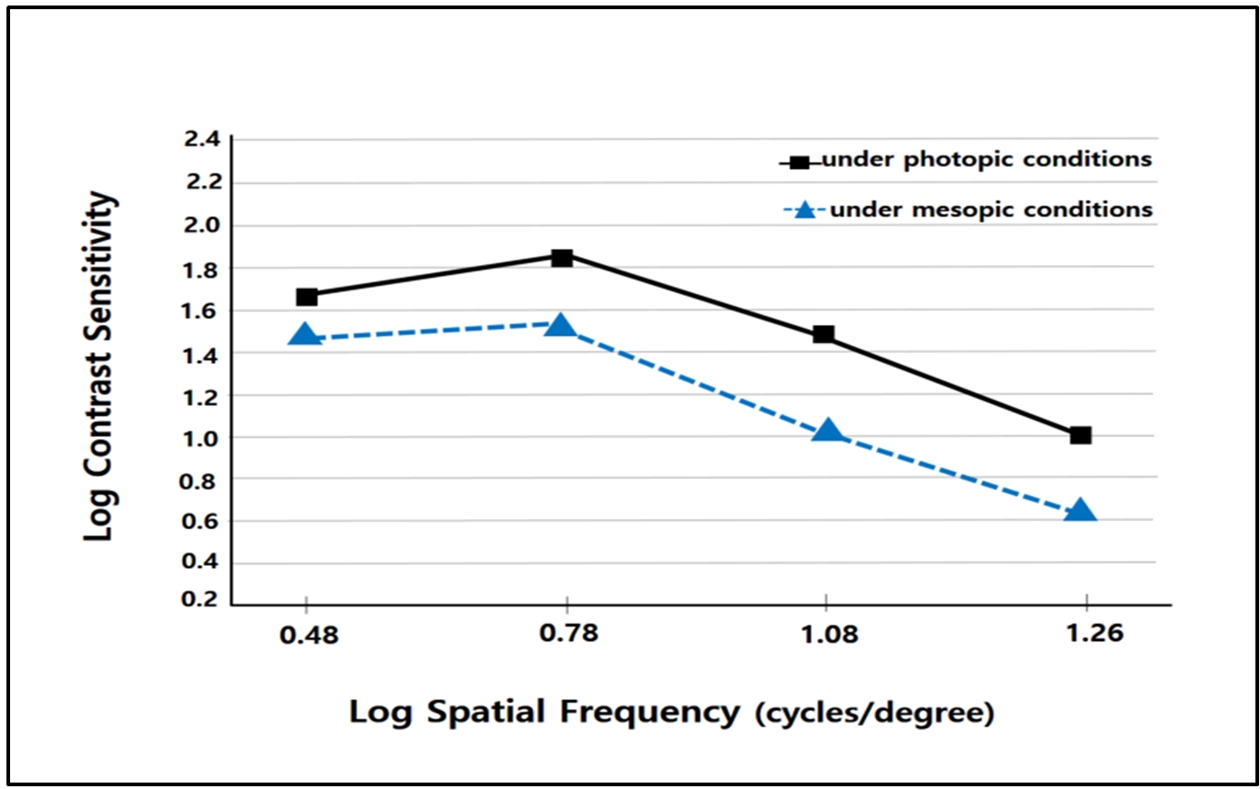
In the LASIK group, the results of log contrast sensitivity at four spatial frequencies (3, 6, 12, and 18 cpd) are shown in Table 2. Additionally, the log contrast sensitivity at four log spatial frequencies according to photopic and mesopic lighting conditions is compared in Fig. 1. This indicates that contrast sensitivity under mesopic lighting conditions decreases at all given spatial frequencies compared to the contrast sensitivity under photopic lighting conditions. The means of the photopic and mesopic AULCSF were 1.28±0.06 (1.06 to 1.40) and 0.99±0.09 (0.79 to 1.12), respectively. There was a significant difference in AULCSF between photopic and mesopic lighting conditions (p<0.001).

Mean of log contrast sensitivity at four spatial frequencies under photopic and mesopic lighting conditions after LASIK
3. Ocular Aberrations and Ocular Scattering
In the ocular aberrations for a 4-mm pupil after LASIK, the means of LOAs, including spherical defocus and astigmatism, were 0.16±0.10 (0.00 to 0.43) and 0.21±0.08 (0.03 to 0.36), and the means of HOAs including total HOAs, coma, spherical aberration were 0.13±0.05 (0.06 to 0.32), 0.09±0.06 (0.00 to 0.26), and 0.03±0.03 (−0.04 to 0.12), respectively. In the optical parameters indicative of retinal image quality, the results of OSI, Strehl ratio, and MTF cut-off after surgery were 0.60±0.37 (0.10 to 1.90), 0.22±0.06 (0.10 to 0.38), and 40.13±9.48 (18.81 to 56.31), respectively.
4. Relationship between AULCSF and Ocular Variables
Correlations between AULCSF and changes in ocular variables after LASIK surgery are summarized in Table 3. Corneal thickness, UCDVA, total HOAs, spherical aberration, and OSI were significantly negatively correlated with the photopic AULCSF (p<0.050), but the MTF cut-off and Strehl ratio showed significantly positive correlations with the photopic AULCSF (p<0.050). Similar to the relationship with the photopic AULCSF, UCDVA, total HOAs, coma, and OSI had significantly negative associations with the mesopic AULCSF (p<0.050), but the MTF cut-off and Strehl ratio showed positive correlations with the mesopic AULCSF (p<0.050).
5. Regression Model between AULCSF and Ocular Variables
The results of the multiple regression analysis after LASIK are presented in Table 4. In the final multiple regression model, independent variables relevant to the photopic AULCSF (R2=0.361, adjusted R2=0.301) were, in order of influence, corrected SE (p=0.021), UCDVA (p=0.021), total HOAs (p=0.030), spherical aberration (p=0.045), and ablation depth (p=0.048). Moreover, independent variables relevant to the mesopic AULCSF (R2=0.326, adjusted R2=0.271) were, in order of influence, OSI (p<0.001), total HOAs (p=0.008), and scotopic pupil size (p=0.031).
Discussion
Many previous studies have reported the effect of LASIK surgery on contrast sensitivity. Some studies reported that photopic contrast sensitivity after LASIK decreased but recovered to normal values at different postoperative times.[12-14,24] In contrast, a previous study found that contrast sensitivity after surgery was depressed and did not return to normal values;[25] moreover, a study using the CSV-1000E under photopic and mesopic lighting conditions reported that contrast sensitivity in LASIK patients was decreased compared with that of the emmetropes.[25]
In this study, it was clearly shown that mesopic contrast sensitivity function decreased at all spatial frequencies compared to the photopic contrast sensitivity function (Table 2). It is commonly assumed that the quality of vision under low lighting conditions deteriorates owing to a decrease in contrast sensitivity. For these reasons, although LASIK patients are highly satisfied with a high-contrast visual acuity chart, they may experience difficulty doing something in medium-to low-contrast environments, including driving at night. Thus, contrast sensitivity testing under different lighting conditions should be conducted to assess subtle changes in visual function after surgery.
With regard to visual acuity, UCDVA was significantly correlated with photopic and mesopic AULCSF, respectively, in the present study (Table 3). In the final multiple regression model, photopic AULCSF in LASIK patients showed statistical significance with UCDVA (Table 4). UCDVA after surgery may be one of the most important metrics for evaluating overall visual performance in clinical practice.[26] Besides, this study found that photopic AULCSF showed statistical significance with ablation depth and corrected SE (Table 4). It is expected that the degradation of contrast sensitivity may be greater because the higher the refractive error to be corrected, the greater is the corneal tissue to be ablated.[14,27] Although there was no significant association between Q-value and AULCSF in this study, corneal asphericity changed from prolate (negative Q-value) to oblate (positive Q-value) after LASIK might play an important role in HOAs, especially spherical aberrations.[28] Therefore, the HOAs response on the cornea after LASIK may depend on the degree of corneal tissue ablation.
In the present study, total HOAs and spherical aberration were significantly correlated with photopic AULCSF (Table 3). In the final multiple regression model, photopic AULCSF showed significance with total HOAs and spherical aberration (Table 4). HOAs including spherical aberration are increased by changing from a prolate to an oblate corneal shape after LASIK.[29,30] It is presumed that the oblate corneal shape after surgery may affect the increase in HOAs and the decrease in visual quality. Previous studies have reported the importance of spherical aberrations related to deteriorating visual quality after LASIK. [5,31] Additionally, Yamane et al. reported that conventional myopic LASIK significantly deteriorated the contrast sensitivity function, despite good UCDVA after surgery.[32] Accordingly, in myopic LASIK, the greater the increase in the magnitude of the achieved myopic correction, the greater is the induced spherical aberration, which may affect the contrast sensitivity.
Considering pupil size, mesopic AULCSF was significantly associated with scotopic pupil size, but photopic AULCSF was not associated with scotopic pupil size in this study (Table 4). Previous studies have reported that the contrast sensitivity function is affected by pupil size.[33,34] The oblate cornea after LASIK may induce HOAs, which will worsen in the dark because the effect of ocular aberrations relies on pupil size.[28,35,36] It has been shown that with greater increase in pupil size, there are more ocular aberrations. As a result, the change in functional vision after LASIK was more significant under lower contrast targets and lower levels of lighting conditions.[28,35]
In reporting the relationship between optical factors and visual quality, most studies have shown a strong influence of ocular HOAs and OSI on contrast sensitivity.[37-39] With regard to optical factors, optical variables, including total HOAs, OSI, MTF cut-off, and Strehl ratio in the current study showed significant correlations with the photopic and mesopic AULCSF, respectively (Table 3). This study agrees with the finding of Marcos,[39] who reported that LASIK causes a decrease in ocular MTF, which accounts for most of the contrast sensitivity reduction. It can be confirmed that the decrease in contrast sensitivity after LASIK is related to optical factors.
As shown in the results, in the final multiple regression model, mesopic AULCSF was significantly associated with total HOAs and OSI (Table 4). As has been reported previously,[39,40] HOAs significantly increased after LASIK, because the larger the refractive error to be corrected, the greater is the corneal tissue to be ablated,[14,27] making the cornea more oblate in shape. Many studies have shown that visual quality is influenced by an increase in ocular HOAs and OSI after LASIK surgery.[4,29,41,42] In addition to this, it is well known that altered corneal shape and irregular corneal surface by laser ablation cause these optical defects.[39,43,44] Ocular scattering is closely related to the PSF (Strehl ratio), which represents the distribution of light on the retinal image corresponding to a point source.[45] It has been clearly shown that the greater the distribution of light scattering, the lower is the quality of the retinal image (Fig. 2).
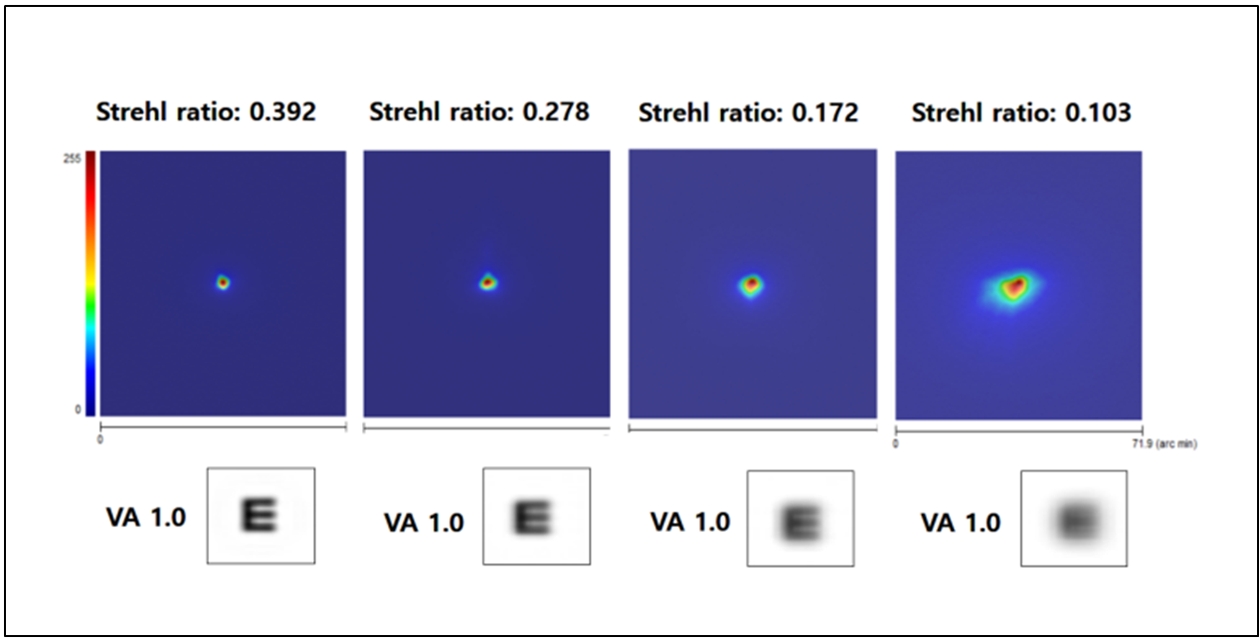
Example of retinal images with 20/20 visual acuity at contrast 100% corresponding to PSF images obtained by OQAS system in subjects who underwent LASIK surgery.
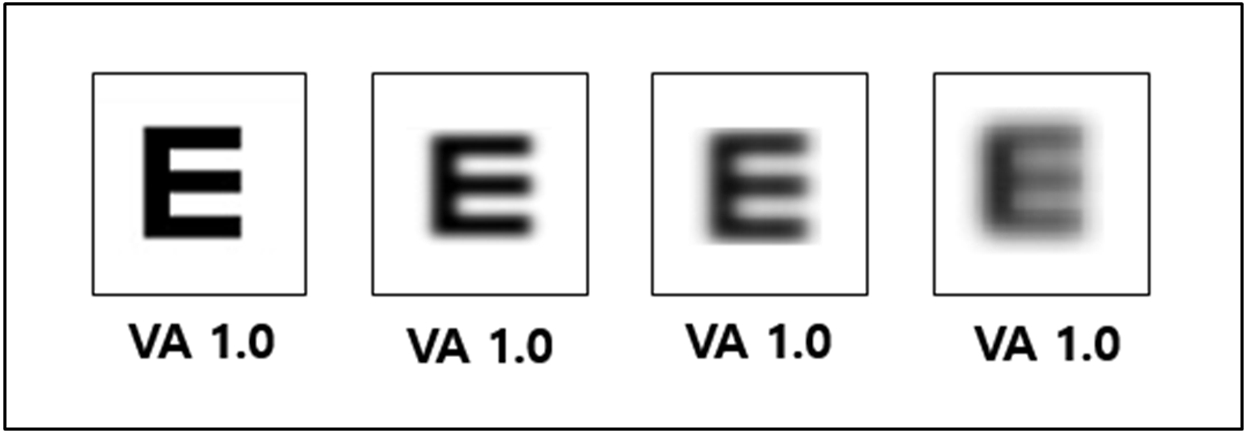
Many studies have shown that a decrease in contrast sensitivity after refractive surgery reduces the quality of visual acuity. In this study, the results are consistent with the fact that contrast sensitivity is affected by multiple factors, and it is also understandable that the optics alone cannot fully explain contrast sensitivity.[26] LASIK patients may have no problems reading or looking at a visual acuity chart with a contrast of 100% under photopic lighting conditions after surgery. As shown in Fig. 3, although LASIK has 20/20 UCDVA on the Snellen visual acuity chart, the spectrum of visual quality for 20/20 visual acuity may be viewed with varying degrees of clarity. These phenomena in the human eye are related to optical aberrations and ocular scattering, resulting in the degradation of retinal image quality in visual function. This can be explained through contrast sensitivity tests under different lighting conditions after surgery. LASIK patients should be reflected in our understanding of the spectrum of visual quality after surgery.
Conclusions
In this study, ocular HOAs and ocular scattering in LASIK patients were shown to be the main factors influencing contrast sensitivity in both photopic and mesopic lighting conditions. LASIK surgery induced significant degradation in contrast sensitivity function under mesopic lighting conditions, although the photopic contrast sensitivity function was close to the normal range. LASIK surgery may adversely affect contrast sensitivity, especially at night, due to these optical factors. Therefore, it is necessary to conduct a contrast sensitivity test under different lighting conditions after LASIK, and providing these visual function tests to patients would be helpful in understanding the quality of their vision at the contrast level encountered in daily life.
References
-
Liang J, Williams DR. Aberrations and retinal image quality of the normal human eye. J Opt Soc Am A. 1997;14(11):2873-2883.
[https://doi.org/10.1364/JOSAA.14.002873]

-
Mrochen M, Semchishen V. From scattering to wavefronts-what’s in between?. J Refract Surg. 2003;19(5):597-601.
[https://doi.org/10.3928/1081-597X-20030901-18]

-
Costello MJ, Johnsen S, Gilliland KO, et al. Predicted light scattering from particles observed in human age-related nuclear cataracts using Mie scattering theory. Invest Ophthalmol Vis Sci. 2007;48(1):303-312.
[https://doi.org/10.1167/iovs.06-0480]

-
McLellan JS, Prieto PM, Marcos S, et al. Effects of interactions among wave aberrations on optical image quality. Vis Res. 2006;46(18):3009-3016.
[https://doi.org/10.1016/j.visres.2006.03.005]

-
Sharma M, Wachler BSB, Chan CCK. Higher order aberrations and relative risk of symptoms after LASIK. J Refract Surg. 2007;23(3):252-256.
[https://doi.org/10.3928/1081-597X-20070301-07]

-
Hosseini SHRJ, Abtahi SMB, Khalili MR. Comparison of higher order aberrations after wavefront-guided LASIK and PRK: one year follow-up results. J Ophthalmic Vis Res. 2016;11(4):350-357.
[https://doi.org/10.4103/2008-322X.194069]

-
Quesnel NM, Lovasik JV, Ferremi C, et al. Laser in situ keratomileusis for myopia and the contrast sensitivity function. J Cataract Refract Surg. 2004;30(6):1209-1218.
[https://doi.org/10.1016/j.jcrs.2003.11.040]

-
Lee YC, Hu FR, Wang IJ. Quality of vision after laser in situ keratomileusis: influence of dioptric correction and pupil size on visual function. J Cataract Refract Surg. 2003;29(4):769-777.
[https://doi.org/10.1016/S0886-3350(02)01844-8]

-
Jindra LF, Zemon V. Contrast sensitivity testing: a more complete assessment of vision. J Cataract Refract Surg. 1989;15(2):141-148.
[https://doi.org/10.1016/S0886-3350(89)80002-1]

-
Heitzmann J, Binder PS, Kassar BS, et al. The correction of high myopia using the excimer laser. Arch Ophthalmol. 1993;111(12):1627-1634.
[https://doi.org/10.1001/archopht.1993.01090120049021]

-
Regan D, Silver R, Murray TJ. Visual acuity and contrast sensitivity in multiple sclerosis-hidden visual loss: an auxiliary diagnostic test. Brain. 1997;100(3):563-579.
[https://doi.org/10.1093/brain/100.3.563]

-
Perez-Santonja JJ, Sakla HF, Alio JL. Contrast sensitivity after laser in situ keratomileusis. J Cataract Refract Surg. 1998;24(2):183-189.
[https://doi.org/10.1016/S0886-3350(98)80198-3]

-
Mutyala S, McDonald MB, Scheinblum KA, et al. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000;107(10):1864-1867.
[https://doi.org/10.1016/S0161-6420(00)00355-9]

-
Chan JWW, Edwards MH, Woo GC, et al. Contrast sensitivity after laser in situ keratomileusis: one-year follow-up. J Cataract Refract Surg. 2002;28(10):1774-1779.
[https://doi.org/10.1016/S0886-3350(02)01499-2]

- Ginsburg AP, Cannon MW. Comparison of three methods for rapid determination of threshold contrast sensitivity. Invest Ophthalmol Vis Sci. 1983;24(6):798-802.
-
Ginsburg AP, Evans DW, Cannon Jr MW, et al. Large-sample norms for contrast sensitivity. Am J Optom Physiol Opt. 1984;61(2):80-84.
[https://doi.org/10.1097/00006324-198402000-00003]

-
Applegate RA, Howland HC, Sharp RP, et al. Corneal aberrations and visual performance after radial keratotomy. J Refract Surg. 1998;14(4):397-407.
[https://doi.org/10.3928/1081-597X-19980701-05]

-
Prieto PM, Vargas-Martin F, Goelz S, et al. Analysis of the performance of the Hartmann-Shack sensor in the human eye. J Opt Soc Am A. 2000;17(8):1388-1398.
[https://doi.org/10.1364/JOSAA.17.001388]

-
Liang J, Grimm B, Goelz S, et al. Objective measurement of wave aberrations of the human eye with the use of a Hartmann-Shack wave-front sensor. J Opt Soc Am A. 1994;11(7):1949-1957.
[https://doi.org/10.1364/JOSAA.11.001949]

-
Saad A, Saab M, Gatinel D. Repeatability of measurements with a double-pass system. J Cataract Refract Surg. 2010;36(1):28-33.
[https://doi.org/10.1016/j.jcrs.2009.07.033]

-
Artal P, Benito A, Perez GM, et al. An objective scatter index based on double-pass retinal images of a point source to classify cataracts. PLoS ONE. 2011;6(2):e16823.
[https://doi.org/10.1371/journal.pone.0016823]

-
Logean E, Dalimier E, Dainty C. Measured double-pass intensity point-spread function after adaptive optics correction of ocular aberrations. Opt Express. 2008;16(22):17348-17357.
[https://doi.org/10.1364/OE.16.017348]

-
Miao H, Tian M, He L, et al. Objective optical quality and intraocular scattering in myopic adults. Invest Ophthalmol Vis Sci. 2014;55(9):5582-5587.
[https://doi.org/10.1167/iovs.14-14362]

-
Montes-Mico R, Charman WN. Choice of spatial frequency for contrast sensitivity evaluation after corneal refractive surgery. J Refract Surg. 2001;17(6):646-651.
[https://doi.org/10.3928/1081-597X-20011101-03]

-
Kim JM. Comparison of contrast visual acuity and contrast sensitivity according to degree of preoperative refractive errors in refractive surgery patients. Korean J Vis Sci. 2018;20(3):269-278.
[https://doi.org/10.17337/JMBI.2018.20.3.269]

-
Kamiya K, Shimizu K, Iijima A, et al. Factors influencing contrast sensitivity function in myopic eyes. PLoS One. 2014;9(11):e113562.
[https://doi.org/10.1371/journal.pone.0113562]

-
Kaiserman I, Hazarbassanov R, Varssano D, et al. Contrast sensitivity after wave front-guided LASIK. Ophthalmology. 2004;111(3):454-457.
[https://doi.org/10.1016/j.ophtha.2003.06.017]

-
Holladay JT, Dudeja DR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg. 1999;25(5):663-669.
[https://doi.org/10.1016/S0886-3350(99)00011-5]

- Moreno-Barriuso E, Lloves JM, Marcos S, et al. Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Invest Ophthalmol Vis Sci. 2001;42(6):1396-1403.
-
Kohnen T, Buhren J. Corneal first-surface aberration analysis of the biomechanical effects of astigmatic keratotomy and a microkeratome cut after penetrating keratoplasty. J Cataract Refract Surg. 2005;31(1):185-189.
[https://doi.org/10.1016/j.jcrs.2004.09.048]

-
Chalita MR, Chavala S, Xu M, et al. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology. 2004;111(3):447-453.
[https://doi.org/10.1016/j.ophtha.2003.06.022]

-
Yamane N, Miyata K, Samejima T, et al. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45(11):3986-3990.
[https://doi.org/10.1167/iovs.04-0629]

-
Strang NC, Atchison DA, Woods RL. Effects of defocus and pupil size on human contrast sensitivity. Ophthalmic Physiol Opt. 1999;19(5):415-426.
[https://doi.org/10.1046/j.1475-1313.1999.00459.x]

-
Oshika T, Tokunaga T, Samejima T, et al. Influence of pupil diameter on the relation between ocular higher-order aberration and contrast sensitivity after laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006;47(4):1334-1338.
[https://doi.org/10.1167/iovs.05-1154]

-
Holladay JT, Lynn MJ, Waring GO, et al. The relationship of visual acuity, refractive error, and pupil size after radial keratotomy. Arch Ophthalmol. 1991;109(1):70-76.
[https://doi.org/10.1001/archopht.1991.01080010072036]

-
Charman WN, Chateau N. The prospects for super-acuity: limits to visual performance after correction of monochromatic ocular aberration. Ophthalmic Physiol Opt. 2003;23(6):479-493.
[https://doi.org/10.1046/j.1475-1313.2003.00132.x]

-
Chalita MR, Xu M, Krueger RR. Correlation of aberrations with visual symptoms using wavefront analysis in eyes after laser in situ keratomileusis. J Refract Surg. 2003;19(6):682-686.
[https://doi.org/10.3928/1081-597X-20031101-13]

-
Chalita MR, Krueger RR. Correlation of aberrations with visual acuity and symptoms. Ophthalmol Clin North Am. 2004;17(2):135-142.
[https://doi.org/10.1016/j.ohc.2004.02.008]

-
Marcos S. Aberrations and visual performance following standard laser vision correction. J Refract Surg. 2001;17(5):596-601.
[https://doi.org/10.3928/1081-597X-20010901-19]

- Kim J. Analysis of corneal higher-order aberrations after myopic refractive surgery. Current Optics and Photonics. 2019;3(1):72-77.
-
Wang J, Thomas J, Cox I. Corneal light backscatter measured by optical coherence tomography after LASIK. J Refract Surg. 2006;22(6):604-610.
[https://doi.org/10.3928/1081-597X-20060601-14]

-
Jain S, Khoury JM, Chamon W, et al. Corneal light scattering after laser in situ keratomileusis and photorefractive keratectomy. Am J Ophthalmol. 1995;120(4):532-534.
[https://doi.org/10.1016/S0002-9394(14)72672-8]

-
Jiménez JR, Anera RG, Del Barco LJ, et al. Retinal image quality in myopic subjects after refractive surgery. J Mod Opt. 2000;47(9):1587-1598.
[https://doi.org/10.1080/09500340008235125]

-
Holladay JT, Janes JA. Topographic changes in corneal asphericity and effective optical zone after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28(6):942-947.
[https://doi.org/10.1016/S0886-3350(02)01324-X]

-
Van den Berg TJTP, Franssen L, Coppens JE. Straylight in the human eye: testing objectivity and optical character of the psychophysical measurement. Ophthalmic Physiol Opt. 2009;29(3):345-350.
[https://doi.org/10.1111/j.1475-1313.2009.00638.x]