
5-Lipoxygenase Mediates Vascular Smooth Muscle Cell Depolarization Induced by 4-hydroxynonenal



Abstract
Retinal neovascularization (NV) is a vision-threatening complication of ischemic retinopathy that develops in various retinal disorders including diabetic retinopathy. To better understand how retinal neovasculari-zation through 4-hydroxynonenal (HNE)-mediated oxidative stress results in a wide range of biological effects, we determined whether the activation of lipoxygenase (LO) by HNE is mediated by reactive oxygen species (ROS) in vascular smooth muscle cells (VSMCs).
A10 cells were incubated with DMEM (0.5% FBS) containing HNE after preincubated for 30 min with various inhibitors. Data were analyzed by flow cytometry and western blot analysis.
High levels of HNE (30 M) induced ROS formation and altered the mitochondrial membrane potential (ΔΨm), ultimately leading to VSMC apoptosis. Pretreatment with nordihydroguaiaretic acid (LO inhibitor), AA 861 (5-LO inhibitor), and baicalin (12-LO inhibitor) prevented HNE-induced ROS generation. AA 861 also blocked the loss of ΔΨm, indicating that LO is closely involved in mitochondria-derived ROS production, thereby leading to apoptosis. At low levels of HNE (1 mM), 5-LO gene expression increased.
These findings suggest that 5-LO mediates HNE-induced VSMC apoptosis by triggering mitochondrial dysfunction and activation by ROS excessive generation leading to the deterioration of vasculature homeostasis and subsequent vascular dysfunction, including retinal NV.
초록
망막 혈관신생(NV)은 당뇨망막병증을 비롯한 다양한 망막장애에서 발생하는 허혈성 망막병증의 시력을 위협하는 합병증이다. 4-hydroxynonenal(HNE) 매개 산화스트레스를 통한 망막 혈관신생을 더 잘 이해하기 위해 본 연구는 HNE에 의한 lipoxygenase(LO)의 활성화가 혈관평활근세포에 있어 활성산소종(ROS)에 의해 매개되는지를 연구하였다.
쥐 대동맥 평활근세포주인 A10 세포를 다양한 억제제와 함께 30분 동안 전처리 한 후 HNE를 함유하는 DMEM(0.5% FBS)에서 배양하였다. 데이터를 Flow cytometry와 Western blot로 분석하였다.
HNE (high level, 30 mM)는 ROS형성과 미토콘드리아 막전위변화를 유도하여 궁극적으로 혈관평활근세포의 세포자살을 유도하였다. LO 억제제, nordihydroguaiaretic acid(NDGA), AA 861(5-LO inhibitor), baicalin(12-LO inhibitor)은 HNE에 의해 유도된 ROS생성을 저해하였다. AA 861는 또한 미토콘드리아 막전위의 손실을 차단하였는데, 이것은 LO가 미토콘드리아 유래 ROS생성에 밀접하게 관여하여 결국 apoptosis을 유도하는 것으로 나타났다. 1 mM HNE (낮은 농도)는 5-LO 유전자 발현 또한 증가 시켰다.
본 연구에서, 이러한 결과는 5-LO는 HNE에 의해 유도되는 미토콘드리아 기능장애와 ROS 과잉생산 유발을 통해 혈관평활근세포의 세포자살을 매개하는 것을 시사한다. 이러한 5-LO의 작용을 통해 혈관계 항상성을 악화시키며 결국 망막 혈관신생과 같은 혈관기능장애에 이르게 하는 것으로 사료된다.
Keywords:
4-Hydroxynonenal, Lipoxygenase, Mitochondrial depolarization, ROS, Retinal neovascularization키워드:
4-하이드록시노네날, 리폭시제네이즈, 미토콘드리아 탈분극, 활성산소종, 망막혈관신생Introduction
Retinal diseases (RD), including diabetic retinopathy, are among the most important eye diseases in industrialized countries. RD is characterized by abnormal angiogenesis associated with an increase in cell proliferation and apoptosis.[1] Angiogenesis in proliferative diabetic retinopathy is a complex multistep phenomenon consisting of the sprouting and the growth of new capillary blood vessels starting from the pre-existing ones.[2] It requires the cooperation of several cell types such as endothelial cells (ECs), vascular smooth muscle cells (VSMCs), which should be activated, proliferate and migrate to invade the extracellular matrix and cause vascular remodeling. [3,4,5]
Retinal neovascularization (NV) is a common cause of vision loss in proliferative diabetic retinopathy, retinopathy of prematurity and age-related macular degeneration (AMD).[6] Recent studies suggested that reactive oxygen species (ROS) play a significant role in pathological angiogenesis.[7] Oxidative stress induced by ROS and reactive nitrogen species (RNS) seem to play a critical role in mitochondrial-associated degradation pathogenesis.[8] Lipid peroxidation induced by ROS/RNS causes formation 4-Hydroxynonenal (HNE) that involved in many processes that are biologically damaged.[9,10]
HNE is end-products and remnants of lipid peroxidation processes that may also act as mediators for the primary free radicals that initiated lipid peroxidation.[11] HNE produced with relatively large amounts is believed to be responsible for the key mediator of oxidative stress-induced cell death. [12] It seems logical that HNE is are the subjects of recent intensified studies investigating their roles in the modulation of cell signaling pathways and the induction of apoptosis. [9,13]
Lipoxygenase (LO) is involved in chronic vascular pathologies, including diabetic retinopathy and age-related macular degeneration.[14,15] LO are regulators of inflammation and oxidative stress formation and enhancers of proliferation in VSMC. [16] Abnormal growth and accumulation of VSMCs within the arterial intima appears a common step in the retinal neovascularization.[17] LO plays an important role in regulating angiogenesis, but the mechanism to date is controversial, even contradictory. [18]
Several actions of the LO pathway may play a role in VSMC activation related in NV. HNE has been suggested to mediate a number of oxidative stress-linked pathological events such as cell proliferation and apoptosis. The goal of this study is delineation the action mechanism of LO in HNE-activated VSMC leading to retinal disorders.
Materials and Methods
1. Culture conditions and HNE treatments
The A10 cells, rat aortic smooth muscle cell line, were obtained from American type culture collection (American type culture collection, USA) and grown in Dulbecco's modified Eagle's medium (DMEM) (Sigma Aldrich, USA) supplemented with 10% fetal bovine serum (FBS), 100 units/ml penicillin and 100 μg/ml streptomycin. Cells were maintained at 37oC in a humidified atmosphere containing 5% CO2/95% air.
For all experiments, cells were seeded at a density of 4 × 104/well into 12-well microplates with DMEM containing 10% FBS and supplements. Cells were allowed to adhere in dish overnight, and then the culture medium was replaced with fresh DMEM (0.5% FBS) containing HNE after pre-incubated for 30 min with various inhibitors. A commercial HNE (purity > 98%) was obtained from Cayman Chemical Inc. (Cayman Chemical Inc, USA), and working solutions of HNE were made in phosphate buffered saline (PBS) immediately before use. Working solutions of HNE (<0.1% ethanol) were made in PBS immediately before use.
2. Measurements of mitochondrial membrane potential (ΔΨm)
The 3,3'-dihexyloxacarbocyanine iodide, DiOC6(3) (Sigma Aldrich, USA), was used as a measure of ΔΨm according to methods described previously. [19,20] In brief, cells grown to sub-confluence on glass cover slips were incubated with HNE. Following stimulation for 3 hr, cells were incubated with 100 nM of the dye for an additional 30 min. Then, cells were washed with PBS. Cellular fluorescence was analyzed flow cytometric analysis(BD FACSLyric, BD Biosciences, USA ).
3. Assay of ROS formation
Intracellular reactive oxygen species (ROS) formation was measured by fluorescenceusing 2,7-dichlorodihydrofluorescein diacetate (DCFH-DA) (Sigma Aldrich, USA), Invitrogen, Molecular probes, a dye that permeates cells where it is trapped as the deesterified free acid, which can then react with ROS to form a highly fluorescent 2,7-dichlorofluorescein (DCF). [21] The cells grown in 12-well plates were loaded with 10M DCFH-DA for 30 min, and then incubated with HNE for 30 min at 37oC. Reactions were stopped by aspiration and cells were trypsinized, collected on ice, and analyzed on flow cytometry. Fluorescence intensity was measured for 10,000 cells in each sample. Results were obtained as histogram plots of cell number versus fluorescence intensity (FL-1), and the mean fluorescence for each sample within an experiment was analyzed as % of total cells.
4. Protein analysis by Western blot analysis
Cells were harvested, washed twice with ice-cold NaCl/P i, and lysed in a TNN buffer (50 m M Tris/HCl, pH 8.0, 120 mM sodium chloride, 0.5% Nonidet P-40) supplemented with protease inhibitors (2 mg/mL-1 aprotinin, 2 mg/mL-1 leupeptin, 100 mg/mL-1 phenylmethanesulfonyl fluoride, 5 lg/mL-1 pepstatin, 1 m M dithiothreitol) and phosphates inhibitors (20 mM NaF, 2 mM Na3VO4)for 1 h on ice, vortexing every 10 min. Lysates were centrifuged at 8000 g for 30 min to remove insoluble material. Protein concentration was determined by the Lowry method using BSA as standard. Equal amounts of protein were separated on 10-15% SDS/PAGE gels. The gels were subsequently transferred onto a nitrocellulose membrane (BIO-RAD, Korea).
Results and Discussions
1. Induction of VSMC mitochondrial depolarization
Lipid peroxidation and its reactive byproducts, like HNE are reported to cause redox-related degenerative processes, including vascular dysfunction. [13,22] 4-HNE has been suggested to mediate a number of oxidative stress-linked pathological events such as cell proliferation and apoptosis.[23] To assess the HNE-induced VSMC activation contained oxidative stress, we analyzed depolarization of mitochondrial membrane ΔΨm is an early event of apoptosis. We monitored changes in ΔΨm by loading mitochondrial with DiOC6(3). The fluorescence intensity analyzed using FACS. As shown in Fig. 1, the quantity of fluorescent profiles decreased as a result of the loss of ΔΨm (see the M2 in Fig. 1) in the cells treated with 30 mM HNE. These observations indicate that HNE induced loss of ΔΨm that may result in apoptosis.
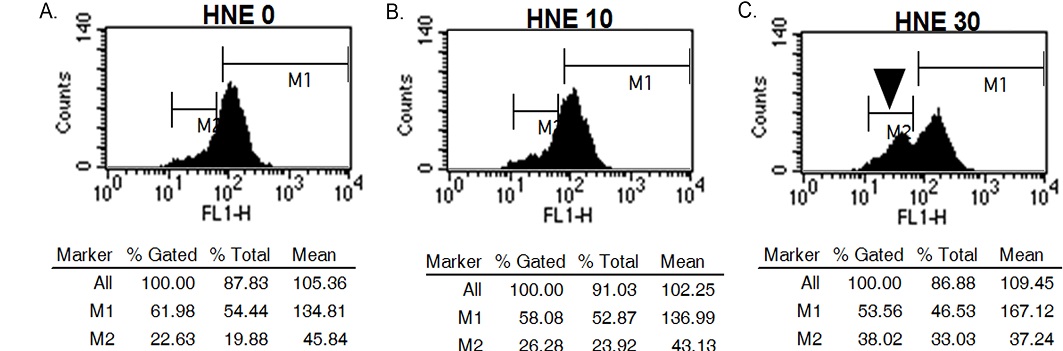
Induction of VSMC mitochondrial depolarization by HNE. Representative histogram plots of cell number versus fluorescence intensity (FL-1). The cells were incubated with HNE for 4 h and then treated with DiOC6(3) for 30 min. The fluorescence intensity was analyzed using FACS. The results were expressed as the percentage of total cells. The quantity of fluorescent profiles decreased due to the loss of ΔΨm in cells treated with 30 μM HNE (M2 indicated by arrowhead).
2. Protection of LO inhibitors against HNE-induced RS formation
Consistent with the reports that lipid oxidation products including HNE and other reactive aldehydes stimulate reactive species (RS) formation in various types of cells. [24] Furthermore, it is well documented and widely known that oxidative stress is a precursor to elevated levels of ROS. [25] Recently, it has become evident that mitochondria are a major source of ROS, and so contribute to redox cell signaling. [26] Furthermore, mitochondria have been considered as an important source of HNE-induced ROS generation since the literatures describing experiments with isolated mitochondria suggest that lipid electrophiles, such as HNE, can modify mitochondrial function. [27]
We monitored protection of LO inhibitors against HNE-induced ROS formation. As shown in Fig. 2, LO inhibitors protected the ROS generation in the cells treated with 30 mM HNE. Pretreatment with LO inhibitor, nordihydroguaiaretic acid (NDGA), AA 861 (5-LO inhibitor), and baicalin (12-LO inhibitor) prevented HNE-induced ROS generation. These observations indicate that HNE induced ROS generation mediated with LO.
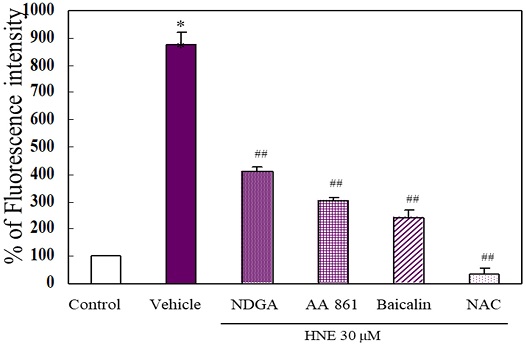
Protection of LO inhibitors against HNE-induced ROS formation. The cells were incubated with 30 μM HNE for 30 min after pretreatment with the antioxidant N-acetylcysteine (NAC, 500 μM) and lipoxygenase inhibitors, nordihydroguaiaretic acid (NDGA, 1 μM, nonspecific), AA 861 (1 μM, 5-LO), and baicalin (1 μM, 12-LO), respectively, with DCF-DA (10 μM) and analyzed using FACS. Data represent the percentage of DCF fluorescence intensity relative to the control. The results are presented as the mean±SEM of three independent experiments. Statistical significance: *p<0.05 vs. control; ##p<0.01 vs. vehicle
3. Inhibitory effects of AA 861 on HNE-induced mitochondrial depolarization
In order to study the action of LO on mitochondrial depolarization induced by HNE, inhibitors were tested to block mitochondrial depolarization. The results showed that HNE (high level, 30 mM) induces ROS formation and alteration of mitochondrial membrane potential (ΔΨm), ultimately leading to VSMC apoptosis(Fig 3). Nonspecific LO inhibitor, NDGA and 12-LO inhibitor bicalin did not prevent HNE-induced depolarization of mitochondrial membrane. A AA 861 also blocked loss of ΔΨm indicating that 5-LO is closely involved in mitochondria-derived ROS production, thereby leading to apoptosis. Based on these results, it is considered that mitochondrial depolarization by HNE is closely related 5-LO.
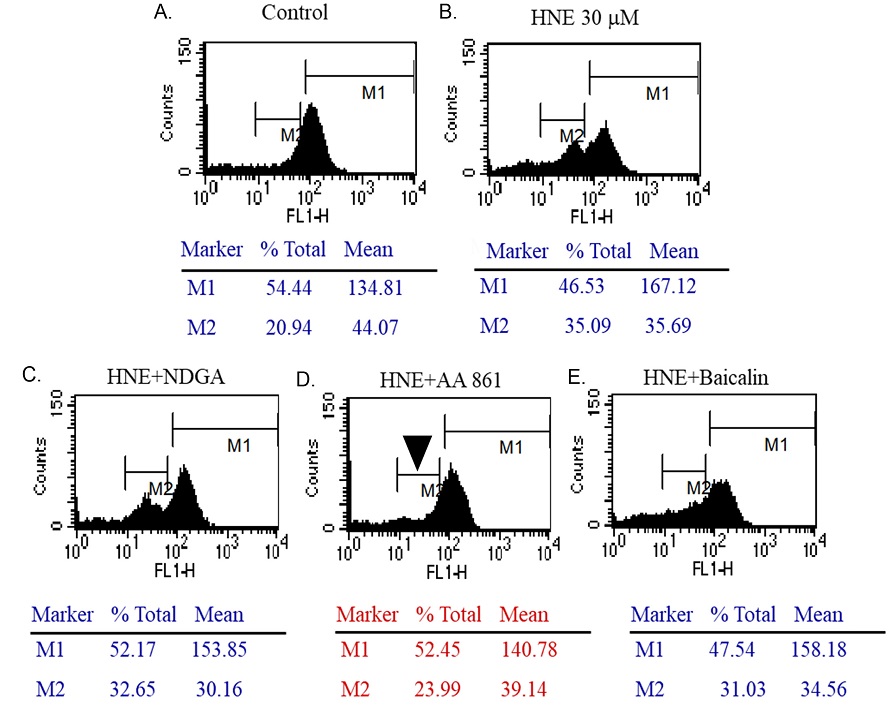
Inhibitory effects of AA 861 on HNE-induced mitochondrial depolarization. Representative histogram plots of cell number versus fluorescence intensity (FL-1). The cells were incubated with 30 μM HNE for 4 h after pretreatment with inhibitors and loaded with DiOC6(3) for 30 min. The fluorescence intensity was analyzed using FACS. The results were expressed as the percentage of total cells. AA 861 (5-LO inhibitor) blocked mitochondrial depolarization induced by HNE (arrowhead).
4. Fig. 4. Up-regulation of VSMC 5-LO expression induced by HNE
In our study, HNE-induced mitochondrial depolarization was found to be associated with LO. Therefore, it was tested whether HNE actually induced expression of 5LO. At 1 mM HNE (Low level), 5-LO gene expression was increased(Fig. 4). These findings suggest that 5-LO mediates HNE-induced VSMC apoptosis by triggering mitochondrial dysfunction and activation by ROS excessive generation leading to the deterioration of vasculature homeostasis and subsequent vascular dysfunction including retinal neovascularization.
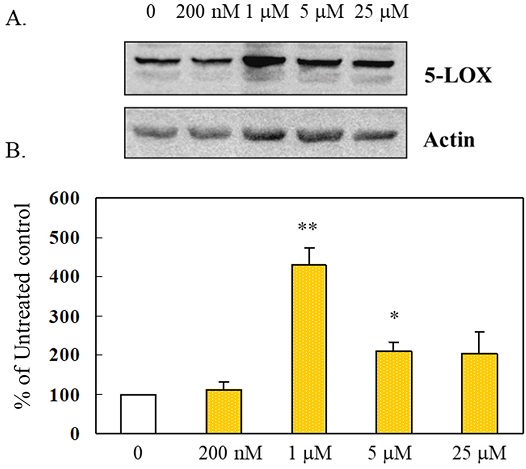
Upregulation of VSMC 5-LO expression induced by HNE. The cells were incubated with HNE for 24 h. 5-LO proteins were analyzed by western blotting. A. Upregulation of 5-LO gene expression by HNE. The data are representative of at least three separate experiments. B. Quantification of 5-LO expression was performed by densitometric analysis. The results are presented as the mean±SEM of three independent experiments. Statistical significance: *p<0.05, **p<0.01, vs. control
HNE is end-products and remnants of lipid peroxidation processes that may also act as mediators for the primary free radicals that initiated lipid peroxidation. [28] HNE produced with relatively large amounts is believed to be responsible for the key mediator of oxidative stress-induced cell death.[10,12] These reactive aldehydes are known to cause redox disturbances and various degenerative processes, including the vascular dysfunction associated with aging.[29] It seems logical that HNE is the subjects of recent intensified studies investigating their roles in the modulation of cell signaling pathways and the induction of apoptosis. [13,23]
Mitochondrial dysfunction caused by chronic exposure to oxidants and increased activation of mitochondrial permeability transition was found to involve mitochondrial depolarization in human aortic endothelial cell apoptosis.[16] Recent study showed that mitochondrial dysfunction in age-related macular degeneration.[30] The enzyme lipoxygenase (LO), which participated in mediating the inflammatory reaction there by retinal change in diabetic retinopathy.[18,31]
Ocular vascular diseases such as diabetic retinopathy, retinal vein occlusion, and age-related macular degeneration, whose population increases along with aging, have become leading causes of severe visual disturbance. HNE is a substance closely related to aging, which increases with aging. Retinopathy is induced by oxygen exposure induced by HNE in several retinal diseases including retinopathy of prematurity, diabetic retinopathy, age-related macular degeneration and central vein occlusion.
However, ROS-dependent HNE’s ability to induce VSMC dysfunction through the regulation of mitochondrial apoptosis is not yet well described. Thus, it is important to define the role of HNE in VSMC apoptosis in relation to mitochondrial dysfunction. The author established that HNE induced the apoptosis of vascular smooth muscle cells through by mitochondrial depolarization. Furthermore, our study show that in VSMC HNE triggers 5-LO gene expression. These findings strongly suggest that 5-LO mediate VSMC apoptosis induced by HNE, leading to vascular dysfunction such as NV.
Conclusions
Taken together, these results suggest that LO mediates HNE-induced VSMC apoptosis by triggering mitochondrial dysfunction and activation by ROS excessive generation leading to the deterioration of vasculature homeostasis and subsequent vascular dysfunction including retinal NV.
Acknowledgments
This work was researched with a grant from the Suseong University research program in 2021.
References
-
Lou H, Kang D, Yang Q, et al. Erythropoietin protects retina against ceramide 2-induced damage in rat. Curr Mol Med. 2017;17(10):699-706.
[https://doi.org/10.2174/1566524018666180322161252]

-
Hendrick AM, Gibson MV, Kulshreshtha A. Diabetic retinopathy. Prim Care. 2015;42(3):451-464.
[https://doi.org/10.1016/j.pop.2015.05.005]

-
Wang L, Bao H, Wang KX, et al. Secreted miR-27a induced by cyclic stretch modulates the proliferation of endothelial cells in hypertension via GRK6. Sci Rep. 2017;7(1):41058.
[https://doi.org/10.1038/srep41058]

-
Orlova VV, Drabsch Y, Freund C, et al. Functionality of endothelial cells and pericytes from human pluripotent stem cells demonstrated in cultured vascular plexus and zebrafish xenografts. Arterioscler Thromb Vasc Biol. 2014;34(1):177-186.
[https://doi.org/10.1161/ATVBAHA.113.302598]

-
Liu S, Lin Z. Vascular smooth muscle cells mechanosensitive regulators and vascular remodeling. J Vasc Res. 2022;59:90-113.
[https://doi.org/10.1159/000519845]

-
Damico FM. Angiogenesis and retinal diseases. Arq Bras Oftalmol. 2007;70(3):547-553.
[https://doi.org/10.1590/S0004-27492007000300030]

-
Nita M, Grzybowski A. The role of the reactive oxygen species and oxidative stress in the pathomechanism of the age-related ocular diseases and other pathologies of the anterior and posterior eye segments in adults. Oxid Med Cell Longev. 2016;3164734.
[https://doi.org/10.1155/2016/3164734]

-
Mehrzadi S, Hemati K, Reiter RJ, et al. Mitochondrial dysfunction in age-related macular degeneration: melatonin as a potential treatment. Expert Opin Ther Targets. 2020;24(4):359-378.
[https://doi.org/10.1080/14728222.2020.1737015]

-
Pedersen WA, Fu W, Keller JN, et al. Protein modification by the lipid peroxidation product 4-hydroxynonenal in the spinal cords of amyotrophic lateral sclerosis patients. Ann Neurol. 2004;44(5):819-824.
[https://doi.org/10.1002/ana.410440518]

-
Lee JY, Jung GY, Heo HJ, et al. 4-Hydroxynonenal induces vascular smooth muscle cell apoptosis through mitochondrial generation of reactive oxygen species. Toxicol Lett. 2006;166(3):212-221.
[https://doi.org/10.1016/j.toxlet.2006.07.305]

-
Uchida K. 4-Hydroxy-2-nonenal: a product and mediator of oxidative stress. Prog Lipid Res. 2003;42(4):318-343.
[https://doi.org/10.1016/S0163-7827(03)00014-6]

-
Awasthi YC, Sharma R, Sharma A, et al. Self-regulatory role of 4-hydroxynonenal in signaling for stress-induced programmed cell death. Free Radic Biol Med. 2008;45(2):111-118.
[https://doi.org/10.1016/j.freeradbiomed.2008.04.007]

-
Lee JY, Je JH, Kim DH, et al. Induction of endothelial apoptosis by 4-hydroxyhexenal. Eur J Biochem. 2004;271(7):1339-1347.
[https://doi.org/10.1111/j.1432-1033.2004.04042.x]

-
Sapieha P, Stahl A, Chen J, et al. 5-Lipoxygenase metabolite 4-HDHA is a mediator of the antiangiogenic effect of omega-3 polyunsaturated fatty acids. Sci Transl Med. 2011;3(69):69-ra12.
[https://doi.org/10.1126/scitranslmed.3001571]

-
Wang MH, Hsiao G, Al-Shabrawey M. Eicosanoids and oxidative stress in diabetic retinopathy. Antioxidants. 2020;9(6):520.
[https://doi.org/10.3390/antiox9060520]

-
Natarajan R, Nadler JL. Lipoxygenases and lipid signaling in vascular cells in diabetes. Front Biosci. 2003;8(6):783-795.
[https://doi.org/10.2741/1144]

-
Scheppke L, Murphy EA, Zarpellon A, et al. Notch promotes vascular maturation by inducing integrin-mediated smooth muscle cell adhesion to the endothelial basement membrane. Blood. 2012;119(9):2149-2158.
[https://doi.org/10.1182/blood-2011-04-348706]

-
Al-Shabrawey M, Mussell R, Kahook K, et al. Increased expression and activity of 12-lipoxygenase in oxygen-induced ischemic retinopathy and proliferative diabetic retinopathy: implications in retinal neovascularization. Diabetes. 2011;60(2):614-624.
[https://doi.org/10.2337/db10-0008]

-
Kataoka M, Fukura Y, Shinohara Y, et al. Analysis of mitochondrial membrane potential in the cells by microchip flow cytometry. Electrophoresis. 2005;26(15):3025-3031.
[https://doi.org/10.1002/elps.200410402]

-
Yang J, Liu X, Bhalla K, et al. Prevention of apoptosis by Bcl-2: release of cytochrome c from mitochondria blocked. Science. 1997;275(5303):1129-1132.
[https://doi.org/10.1126/science.275.5303.1129]

-
Cathcart R, Schwiers E, Ames BN. Detection of picomole levels of hydroperoxides using a fluorescent dichlorofluorescein assay. Anal Biochem. 1983;134(1):111-116.
[https://doi.org/10.1016/0003-2697(83)90270-1]

-
Usatyuk PV, Natarajan V. Role of mitogen-activated protein kinases in 4-hydroxy-2-nonenal-induced actin remodeling and barrier function in endothelial cells. J Biol Chem. 2004;279(12):11789-11797.
[https://doi.org/10.1074/jbc.M311184200]

-
Nègre-Salvayre A, Garoby-Salom S, Swiader A, et al. Proatherogenic effects of 4-hydroxynonenal. Free Radic Biol Med. 2017;111:127-139.
[https://doi.org/10.1016/j.freeradbiomed.2016.12.038]

-
Knöbel Y, Glei M, Osswald K, et al. Ferric iron increases ROS formation, modulates cell growth and enhances genotoxic damage by 4-hydroxynonenal in human colon tumor cells. Toxicol In Vitro. 2006;20(6):793-800.
[https://doi.org/10.1016/j.tiv.2005.11.009]

-
Galaris D, Barbouti A, Pantopoulos K. Iron homeostasis and oxidative stress: an intimate relationship. Biochim Biophys Acta Mol Cell Res. 2019;1866(12):118535.
[https://doi.org/10.1016/j.bbamcr.2019.118535]

-
Diebold L, Chandel NS. Mitochondrial ROS regulation of proliferating cells. Free Radic Biol Med. 2016;100:86-93.
[https://doi.org/10.1016/j.freeradbiomed.2016.04.198]

-
Landar A, Zmijewski JW, Dickinson DA, et al. Interaction of electrophilic lipid oxidation products with mitochondria in endothelial cells and formation of reactive oxygen species. Am J Physiol Heart Circ Physiol. 2006;290(5):1777-1787.
[https://doi.org/10.1152/ajpheart.01087.2005]

-
Chapple SJ, Cheng X, Mann GE. Effects of 4-hydroxynonenal on vascular endothelial and smooth muscle cell redox signaling and function in health and disease. Redox Biol. 2013;1(1):319-331.
[https://doi.org/10.1016/j.redox.2013.04.001]

-
Yu BP, Chung HY. Oxidative stress and vascular aging. Diabetes Res Clin Pract. 2001;54(2):73-80.
[https://doi.org/10.1016/S0168-8227(01)00338-2]

-
Kaarniranta K, Uusitalo H, Blasiak J, et al. Mechanisms of mitochondrial dysfunction and their impact on age-related macular degeneration. Prog Retin Eye Res. 2020;79:100858.
[https://doi.org/10.1016/j.preteyeres.2020.100858]

-
Gubitosi-Klug RA, Talahalli R, Du Y, et al. 5-Lipoxygenase, but not 12/15-lipoxygenase, contributes to degeneration of retinal capillaries in a mouse model of diabetic retinopathy. Diabetes. 2008;57(5):1387-1393.
[https://doi.org/10.2337/db07-1217]
